Background: Currently, there are over 50,000 practicing hospitalists. As it remains a popular career choice for graduating residents, the field has seen a rapid rise in the number of junior faculty. However, there continues to be a gap in those who have advanced to senior academic rank, namely associate or full professor. It is well established that mentorship can play an integral role in career advancement [1-4]. With the dearth of senior faculty, however, dyadic mentoring poses a challenge. Peer mentoring is a feasible option to fill this need [5-7].
Purpose: Our hospital medicine program mirrors those across the country with a disproportionately high number of junior and relatively few senior faculty. We developed a facilitated peer mentoring program with its own dedicated curriculum to educate hospitalists on the purpose of peer mentoring, resources for career advancement, and types of scholarly activities that may be more achievable for busy clinicians. We aimed to create peer groups each guided by a senior member and determine feasibility of the program based on participation. Other objectives, assessed using a pre- and post-program survey, evaluated knowledge improvement of curriculum topics, satisfaction with the program, and whether members felt participation would assist in career advancement. The study was approved by our IRB.
Description: We recruited 29 junior faculty and created five small groups each guided by one senior faculty. Two of the authors designed and presented a dedicated curriculum that included four sessions: 1) Intro to Facilitated Peer Mentorship and Identifying Career Goals, 2) Building a CV Focused on Incorporating Hospitalist Activities, 3) Developing an Educational and Patient Care Portfolio, and 4) Strategies for Hospitalists to Achieve Scholarly Success. Each session was presented to all members in a large group setting. Our aim was to have the small groups meet individually after each large group session so the peer members could review, begin work on previously presented topics, and have the senior facilitator available to answer questions. All sessions occurred over 10 months with alternating large and small group sessions.
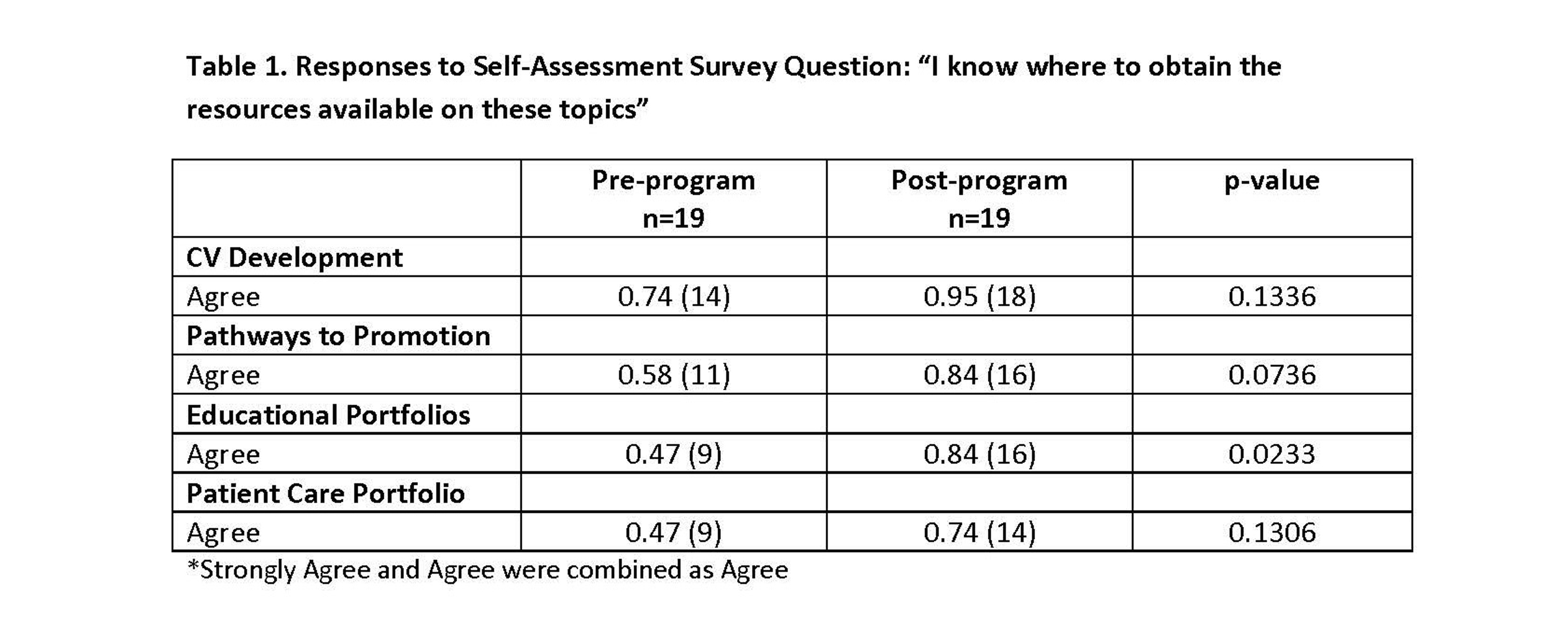
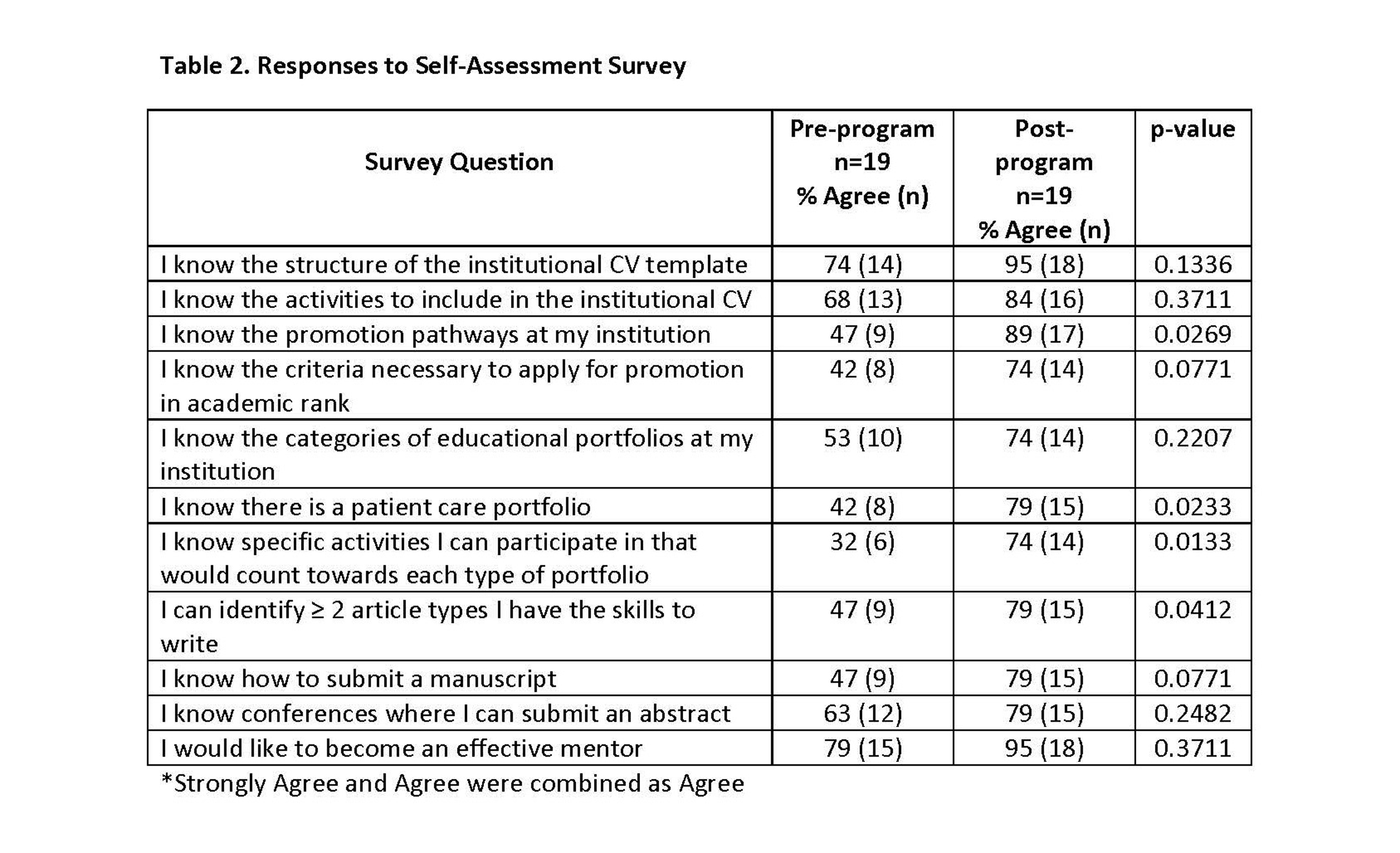
Conclusions: We aimed to achieve an average participation rate of at least 50% in the large and small group sessions to assess feasibility of the program. The average participation rate for the large group sessions was 57.4% which was significantly greater than 50% (p=0.0419). The participation in the small groups was more variable. One group did meet three times and participation in all the sessions was >50%. Another group met once with all members in attendance. The facilitator then met individually with two of the more engaged members throughout the study period. One senior facilitator met individually with three of his peer members citing schedule as barriers to meeting all together. The other two groups were unsuccessful in meeting citing schedule and time as barriers. The surveys demonstrated significant knowledge improvement (p< 0.05) in pathways to promotion, patient care and educational portfolios, activities that would count towards each portfolio type, and articles they have the skills to write. Moreover, 84% of participants were satisfied with the program, 89% felt participation would help in career advancement, and 95% would recommend the program to their colleagues. Our peer program with a dedicated curriculum can hopefully be a bridge to achieving a more even distribution of academic rank amongst hospitalists.