Background:
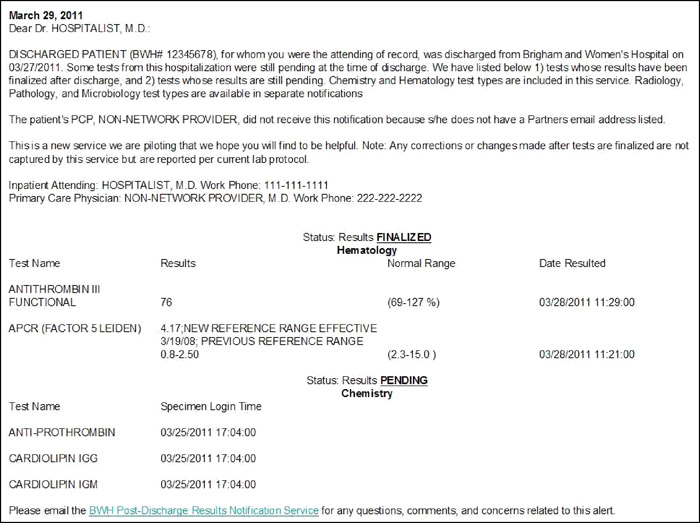
Physician awareness of the results of tests pending at discharge (TPADs) is poor. We developed an automated e‐mail notification system to prompt the inpatient attending and primary care physician (PCP) of TPAD results. The objective of this study is to report the impact of this system on the awareness of finalized TPAD results by responsible physicians. We previously submitted an abstract (HM11, Abstract 36) based on an interim analysis; this abstract represents the completed data set.
Methods:
We performed a cluster‐randomized controlled trial in which both the inpatient attending and network and out‐of‐network PCPs were randomized to the notification system or usual care for patients discharged from inpatient general medicine and cardiology services at Brigham and Women's Hospital. A total of 441 patients discharged by the inpatient attending during the study period were assigned to intervention or usual care if both the inpatient attending and PCP were in the concordant arms of the study. We e‐mailed Web‐based surveys to the inpatient attendings and network PCPs approximately 72 hours after the last TPAD was finalized. Out‐of‐network PCPs and any network physician who did not respond to the initial Web‐based survey were faxed surveys. We measured awareness (dichotomous variable) of any TPAD result by inpatient attending as the primary outcome. We measured awareness of any TPAD result by PCP, awareness of actionable TPAD results, and satisfaction with system (5‐point Likert scale) as secondary outcomes. We performed Fisher's exact test to compare outcomes.
Results:
We received 139 and 136 completed surveys from inpatient attendings, and 69 and 83 completed surveys from PCPs on 241 intervention and 200 control patients, respectively (inpatient attending response rate, 62%; PCP response rate, 34.5%). Inpatient attendings and PCPs were significantly more aware of any TPAD result in the intervention versus usual care arms (inpatient attending awareness: 76% vs. 38%, OR [3.08–8.74]; P < 0.0001; PCP awareness: 57% vs. 33%, OR, 2.7 [1.39–5.22]; P = 0.003). Inpatient attendings were significantly more aware of actionable TPAD results in the intervention versus usual care arms (59% vs. 29%, OR, 3.64 [1.18–11.18]; P = 0.02). Eighty‐nine percent and 70% of intervention inpatient attendings and PCPs, respectively, were satisfied with automated e‐mail notification of TPAD results.
Conclusions:
Awareness of finalized TPAD results under usual care is still poor. Inpatient attendings and network PCPs receiving automated e‐mail notifications were significantly more aware of TPAD results. Inpatient attendings were also more aware of actionable TPAD results. Intervention inpatient attendings and network PCPs were highly satisfied with automated e‐mail notification of TPAD results. The study was limited by small sample size. This intervention is a promising approach that should be considered for more widespread use to improve management of TPADs in the context of an institution's clinical information systems.
Primary and Secondary Outcomes
| Survey Respondent | Intervention | Control | Crude OR (95% CI), P Value |
| Primary outcome: Awareness of any TPAD results by inpatient attending | |||
| Inpatient attendings aware, % (n) | 76% (106/139) | 38% (52/136) | 5.19 (3.08–8.74), < 0.0001 |
| Hospitalist | 80% (76/95) | 36% (31/86) | 7.10 (3.64–13.8), < 0.0001 |
| Nonhospitalist* | 72% (28/39) | 43% (20/47) | 3.44 (1.39–8.50), 0.007 |
| Secondary outcome: Awareness of any TPAD results by PCP | |||
| PCPs aware, % (n) | 57% (39/69) | 33% (27/83) | 2.70 (1.39–5.22), 0.003 |
| Network PCP | 65% (35/54) | 33% (24/73) | 3.76 (1.79–7.90), 0.0004 |
| Nonnetwork PCP | 18% (2/11) | 29% (2/7) | 0.56 (0.06–5.24), 0.61 |
| Secondary outcome:Awareness of actionable TPAD results‡ | |||
| Inpatient attendings aware, % (n) | 59% (16/27) | 29% (8/28) | 3.64 (1.18–11.18), 0.02 |
| PCPs aware, % (n) | 65% (13/20) | 48% (13/27) | 2.00 (0.61, 6.57), 0.25 |
| *Traditional internists, cardiologists, other subspecialists; ‡TPADs were determined to be actionable by the surveyed physician. |