Background: Communication between patients, nurses and physicians is vital to patient care. Prior studies have shown that a substantial number of hospitalized patients do not understand their care plan and that physician-nurse co-location or time spent communicating have little impact on physician-nurse concordance of plan of care. To our knowledge, there have been no prior studies evaluating the relationship between hospitalist participation in interdisciplinary rounds (IDR) and concordance of care plan between physicians, nurses and patients. In our health system, IDR were conducted by a core group of team members including nurse, nurse leader, care manager, pharmacist (CIDR). As we co-located hospitalists on units, hospitalists participated in IDR (HIDR) on the majority of patients. We hypothesized that HIDR improve concordance over CIDR given that plan of care information originates largely from physicians.
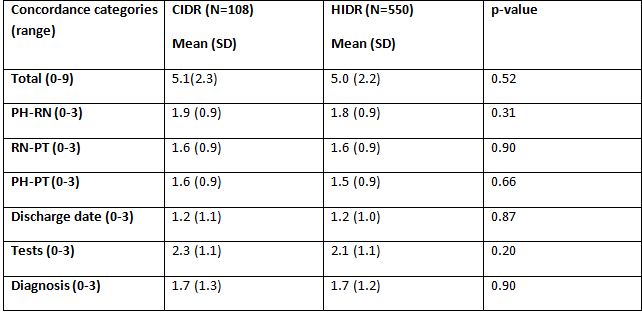
Methods: In this prospective cohort study, we included adult patients admitted to hospitalist services on four units with varying proportions of HIDR and CIDR. Following IDR, we evaluated concordance across three knowledge domains (predicted discharge date, diagnosis, and tests and procedures) and three relationships (Physician-Nurse, Physician-Patient, and Nurse-Patient) using a survey tool. A total concordance score (range 0-9), knowledge domain subgroup score (0-3) and relationship subgroup score (0-3) was calculated for each patient. We also collected data on patient characteristics including demographics, illness severity, admission status, unit, hospitalist group (private versus employed), and payer. We compared demographic characteristics, total and subgroup concordances between IDR groups.
Results: 658 patients were included in the final analysis. Patient characteristics were distributed evenly across IDR groups. 166, 272 and 220 patients were in the ranges of total concordance 0-3, 4-6 and 7-9, respectively. In unadjusted analyses, total and subgroup concordance scores were not different between CIDR and HIDR groups (Table 1).
Conclusions: A substantial number of patients had low total and subgroup concordance that did not change with HIDR. Physician-patient interactions occur once or twice a day and nurse-patient interactions occur 24 or more times a day given hourly rounding. Therefore, physician-nurse agreement may be the stepping stone to physician-nurse-patient agreement due to several opportunities for knowledge sharing between nurses and patients. While we must continue to improve physician-patient interactions in hospital medicine, we recommend focusing future IDR interventions on improving physician-nurse concordance not only during day (IDR) shift, but through the continuum of hospital care.