Background:
Clostridium difficile–associated diarrhea (CDAD) increases the risk of hospital mortality. Factors associated with recurrence of CDAD in clinical trials include renal impairment (RI), inflammatory bowel disease (IBD), and advanced age (>65 years old). These factors may also affect mortality risk. How these factors modify the effect of CDAD on mortality is unknown. Failure to consider interaction effects may result in inaccurate mortality estimates. This cohort study analyzed these effects among hospitalized patients with hospital‐origin CDAD (HO‐CDAD) and community‐origin CDAD (CO‐CDAD) versus non‐CDAD controls.
Methods:
A retrospective analysis (April 2005–June 2011) of the Health Facts® database (Cerner Corp., Kansas City, MO), containing detailed clinical records from 186 U.S. hospitals, identified hospitalized adult patients with a positive C. difficile toxin collected ≥ 48 hours (HO‐CDAD) or < 48 hours (CO‐CDAD) after admission. IBD was defined by diagnosis code, RI by diagnosis code and eGFR. Generalized estimating equation models measured the effects of HO‐ and CO‐CDAD, risk factors (RI, IBD, age > 65), and their interactions, along with other covariates, on hospital mortality.
Results:
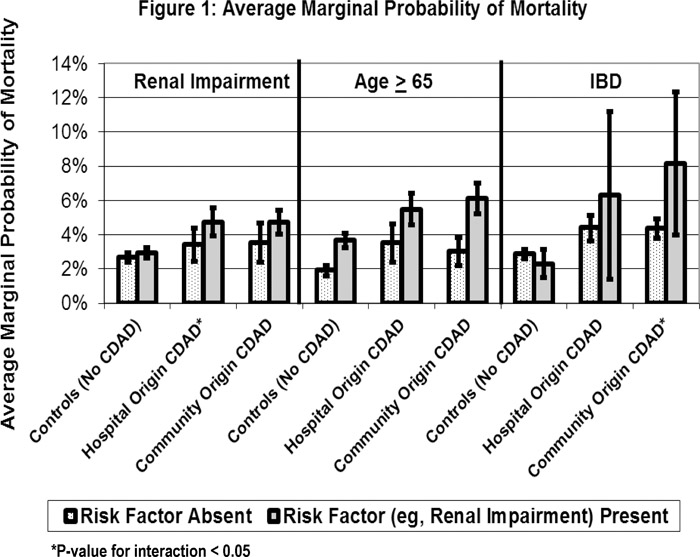
Four thousand five hundred and five patients with HO‐CDAD, 2825 with CO‐CDAD, and 276,486 controls were identified. Unadjusted hospital mortality was 13.0% in HO‐CDAD, 10.7% in CO‐CDAD, and 2.7% in controls. Age > 65 years did not modify the likelihood of mortality in CDAD patients: the odds were approximately doubled across groups regardless of CDAD status. However, the effect of RI on mortality in HO‐CDAD was 1.35 times higher than that in controls (interaction OR, 1.35; 95% CI, 1.01–1.79). Taking the interaction term into account, the overall OR of dying with RI and HO‐CDAD was 1.48 (95% CI, 1.12–2.00). Among controls, IBD had no significant effect on mortality (OR, 0.77; 95% CI, 0.52–1.14). However, the interaction term for CO‐CDAD and IBD was 3.05 (95% CI, 1.20–7.79), for an overall OR for CO‐CDAD with IBD of 2.36 (95% CI, 1.08–5.14). Average marginal probabilities of mortality are in Figure 1.
Conclusions:
The effect of RI and IBD on mortality varies by CDAD status. RI and IBD have a synergistic (multiplicative instead of additive) effect with CDAD on mortality; if patients develop CDAD, their risk of dying greatly increases versus controls. Although age > 65 significantly increases mortality by roughly twofold, its effect was constant across all subgroups.