Background: Hospitalization provides an opportunity to provide patients who use tobacco with evidence-based treatment for cessation, including nicotine replacement therapy, motivational interviewing, and pharmacotherapy. However, this benefit is often lost without appropriate transitions in care to outpatient cessation resources. We have found that inpatient tobacco cessation interventions at our 600-bed urban academic medical center do not result in prolonged tobacco cessation six weeks after discharge, and are attempting to bridge this gap by improving smoking cessation interventions in the period following hospital discharge.
Purpose: We sought to bridge the gap in sustaining inpatient tobacco cessation interventions after discharge by developing an interactive voice response system phone call program that targeted tobacco users after hospital discharge to help address difficulties in sustaining tobacco use treatment after patients leave the hospital.
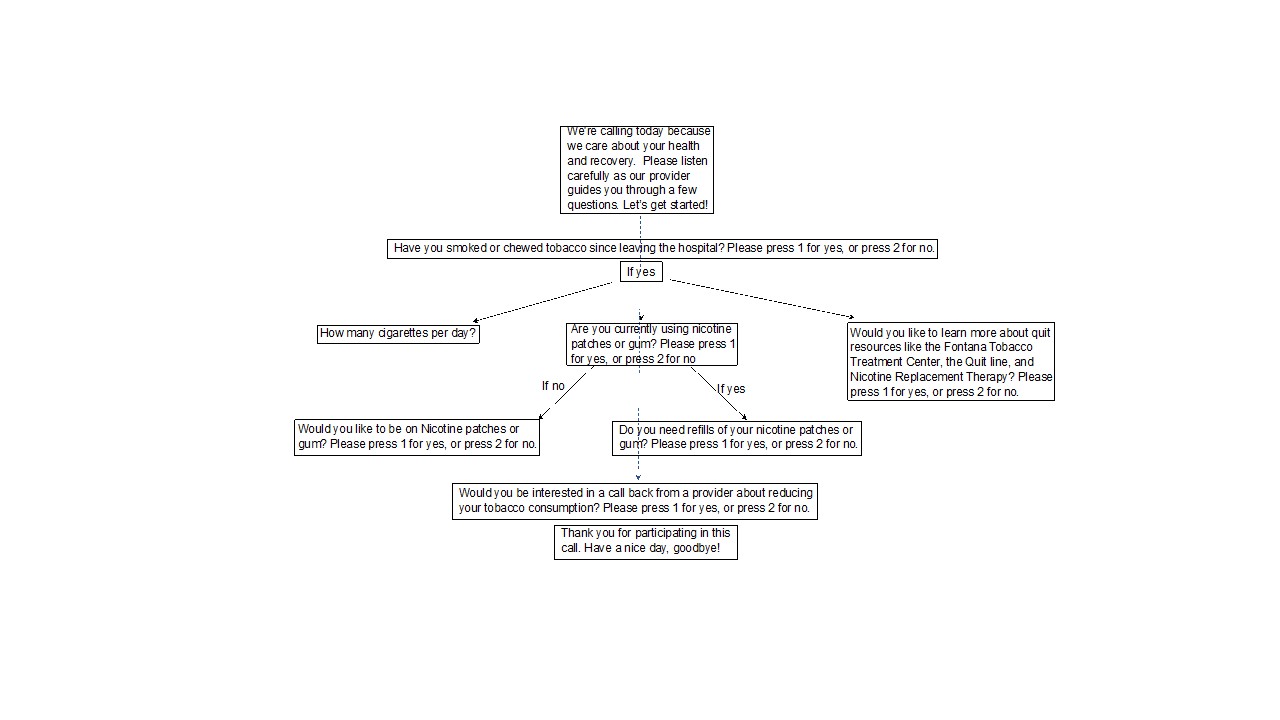
Description: Patient IdentificationPatients’ tobacco use status is part of the nursing admission assessment at our institution, and a smoking cessation inpatient team staffed by respiratory therapists and led by a hospitalist sees approximately 55% of all patients who screen positive for tobacco use and provides these patients with cessation interventions. Through our program, automated phone calls were deployed to all patients with a positive tobacco screen, whether or not they received inpatient smoking cessation team services. Program DescriptionThe automated call used an interactive voice response system to assess whether patients were continuing to use tobacco, quantify the tobacco use, and determine whether nicotine replacement, pharmacotherapy and other outpatient resources had been accessed (Figure 1). If the patients had not received desired resources, were newly interested in these resources, or wanted to talk to a provider about tobacco cessation for any other reason, the hospitalist leading the Smoking Cessation Team would call them. During the first 8 months of the program, a total of 1,075 patients were automatically called with a 69% reach rate, and 194 received follow-up phone calls. Of the patients who asked for a call back, 35% needed assistance with initiating nicotine replacement therapy, 30% asked for other cessation resources, and 35% wanted a call back for another question about tobacco cessation.
Conclusions: An interactive voice response after-discharge phone call for tobacco use is a potentially effective mechanism for continuing inpatient cessation interventions and strengthening linkages to outpatient resources for patients who use tobacco.