Background: In March 2019, the CEO of our public teaching hospital set a goal for the institution to become a high reliability organization. At that time, the hospital’s rates of catheter associated urinary tract infections (CAUTIs), central line associated blood stream infections (CLABSIs), and hospital acquired pressure injuries (HAPIs) were above the national average. Evaluation of current practices at our institution revealed opportunities to improve how patients at risk of harm events were identified and how risks could be reduced. The evaluation also showed that nursing units lacked sufficient management tools to accomplish this task. One management tool that has shown to improve teamwork and anticipatory guidance is a team huddle. Huddles increase situational awareness of staff and allow for timely and coordinated intervention on critical areas of focus. As a result, the Unit Safety Huddle (USH) was implemented and used to identify and immediately remove risks of harm through coordinated intervention.
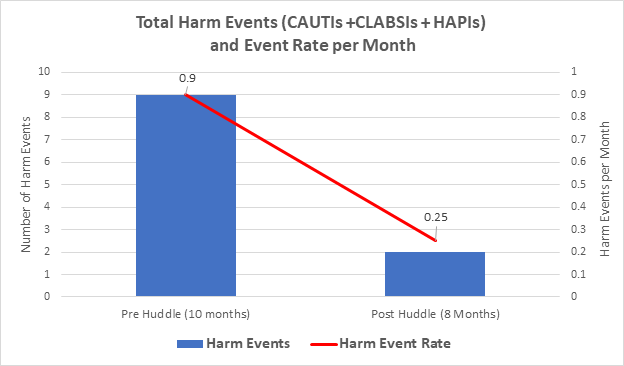
Purpose: To decrease the total event rate of CAUTIs, CLABSIs, and HAPIs from 0.9 per month to 0.5 per month by using unit safety huddles.
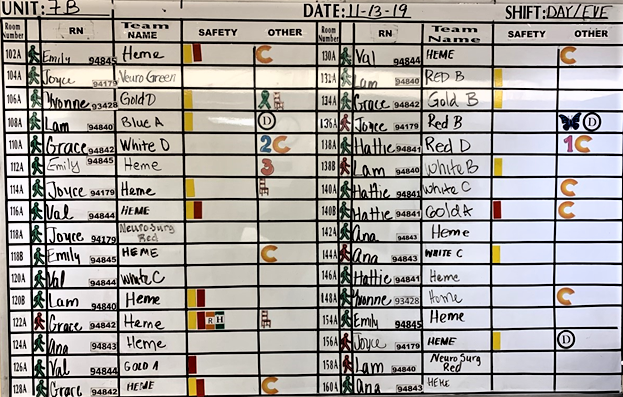
Description: The USH was first piloted on a thirty-two bed medical-surgical unit. The huddles occur daily and are led by frontline nurses and attended by unit nursing staff, nurse leadership, hospital administration, and physicians. Using a standardized script, the huddle facilitator helps the staff identify patients at risk of harm and discusses interventions to keep patients safe. To augment the huddles, an existing white board was repurposed to visually identify patients at risk of CAUTIs, CLABSIs, and HAPIs by using differed colored magnets (Fig 1). After creating colored magnets to represent risk of harm events, the staff further tailored their board to highlight additional risks important to their respective unit (E.g., Green stick figures to represent patients who can ambulate at baseline). We then tracked the number of harm events that occurred before and after the launch of the USH and huddle board.
Conclusions: Following the implementation of the USH, the pilot unit saw a marked reduction in the total number of CAUTIs, CLABSIs, and HAPIs (Fig 2), and the rate of harm events dropped to 0.25 per month. Given the dramatic reduction in harm rate on the pilot unit, we have spread to three additional units, with plans to spread to six more in the next few months. The safety huddles have promoted a culture of teamwork, communication, and transparency. With the safety boards, staff can quickly understand the safety risks for each patient and proactively intervene. Institutional support for patient safety is also evident by the representation of multiple levels of leadership at the huddles. The plan is to continue spreading safety huddles to all the inpatient units to build a framework for safe and reliable care as our hospital continues its journey towards becoming a high reliability organization.