Background: Catheter associated urinary tract infections (CAUTI) are one of the most common hospital acquired infections and cost on average $13,793 per case according to the AHRQ. Many quality and safety organizations including the Society of Hospital Medicine recommend reducing the prevalence of indwelling urinary catheters (IUC) as a means to reduce the incidence of CAUTIs.
Purpose: We sought to reduce IUC usage and as a result reduce CAUTI in our health system using indication-based ordering combined with a nurse-driven removal protocol.
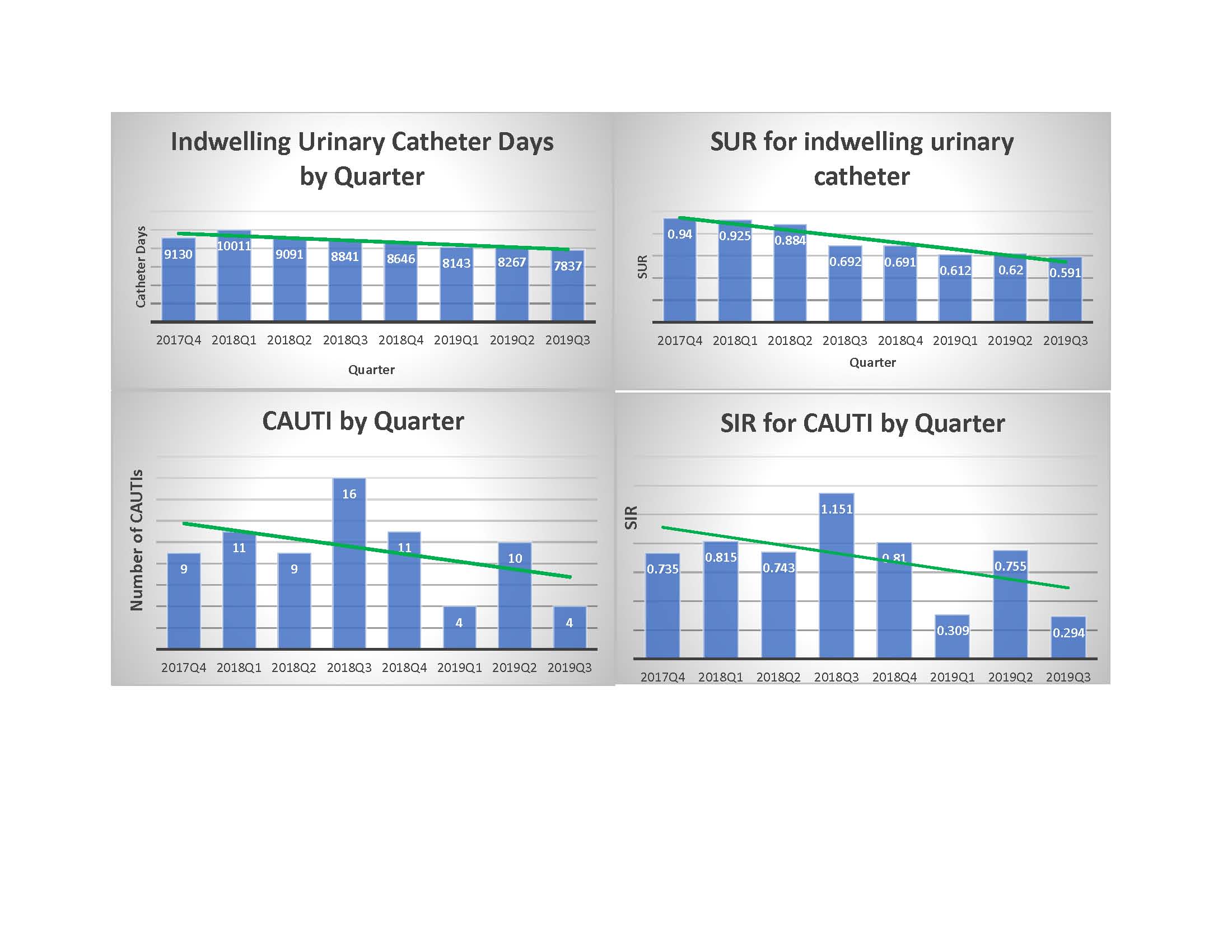
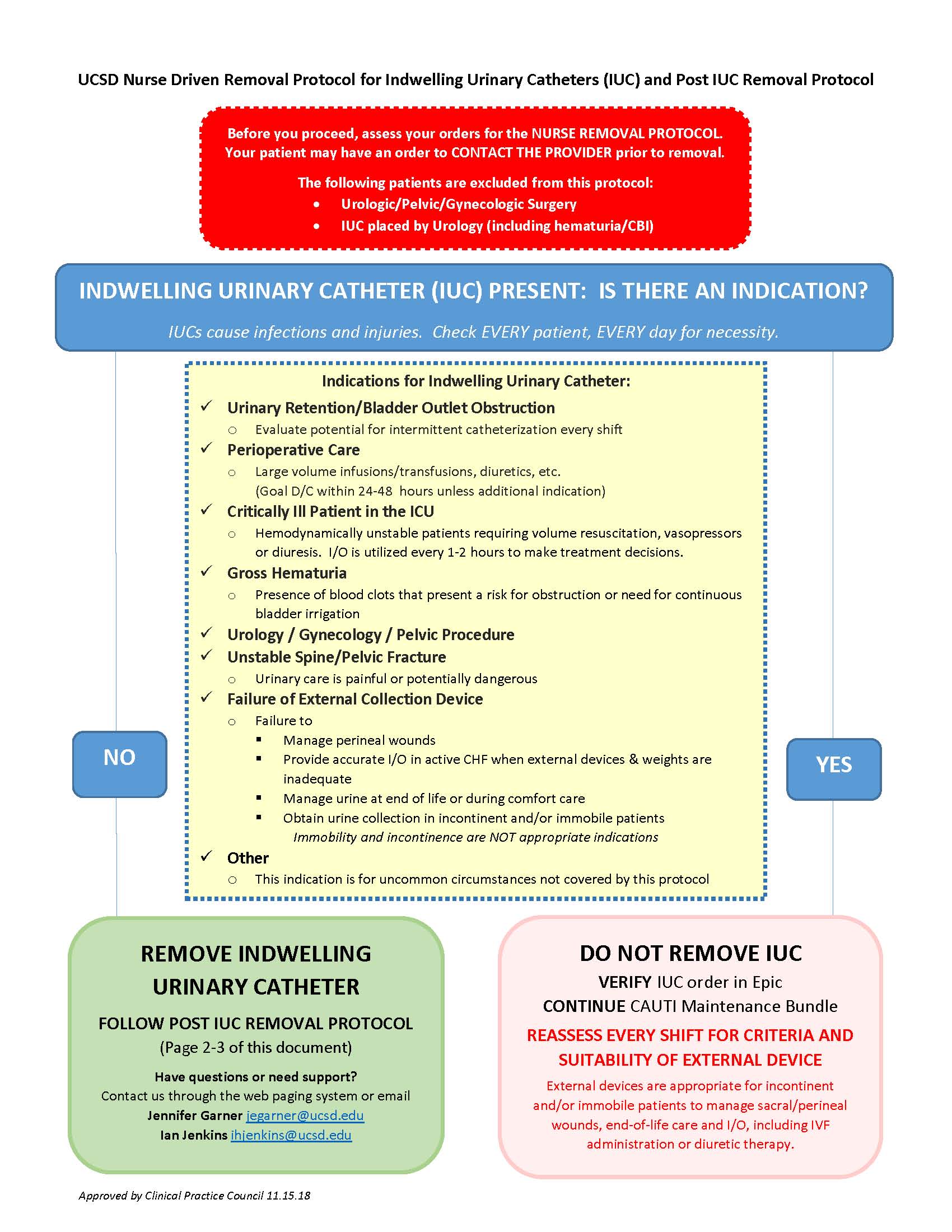
Description: A multidisciplinary team with representatives from hospital medicine, urology, critical care, nursing and informatics developed two tools aimed at reducing overall IUC usage. We created a new indication based urinary management order-set. This order-set required providers to first identify the reason for urine management, then pointed them to appropriate means. For appropriate indications external collection devices or in-and-out catheterizations were prioritized, and IUC usage was limited to appropriate indications based on a combination of guidelines and consensus of the involved stakeholders. We recommended external collection devices for perineal wound healing, incontinence, urine collection, and end of life comfort. The allowed indications for IUC were brief perioperative care, urine output measurement in a critically ill patient, gross hematuria, urology/gynecology/pelvic procedure, unstable spine/pelvis, failure of external urinary collection device, or urinary retention (with the caveat that in-and-out catheterization is preferred). Providers were also allowed to select “other” as an indication for an IUC but had to specify their reason. Once appropriate indications for IUC had been determined, then stakeholders determined by consensus which indications were amenable for utilizing a nurse-driven removal protocol and which indications required a physician order for catheter removal. The only indications that the nurse-driven removal protocol did not apply to and required a physician order to remove were gross hematuria and urology/gynecology/pelvic procedure. The order-set was placed into use in December of 2018. We supported the initiative with physician and nurse training sessions, fliers, nurse champion outreach, and feedback, but efforts were not intensive.Institution-wide IUC days fell from an average of 9143 IUC days in the 5 quarters prior to implementation to an average of 8082 IUC days per quarter after implementation. The average standardized utilization ratio (SUR; observed over expected utilization) fell from 0.83 before implementation to 0.61 following implementation. Our institutional CAUTI rate fell from an average of 11 CAUTIs per quarter in the 5 quarters prior to implementation to an average of 6 CAUTIs per quarter afterwards. The average standardized infection ratio (SIR; observed over expected CAUTIs) fell from 0.85 prior to implementation to 0.45 following implementation.
Conclusions: The combination of indication-based ordering for urine collection management along with the institution of a nurse-driven removal protocol was associated with fewer IUC days and an improved IUC SUR and CAUTI rate/SIR. Our approach may be useful to other institutions attempting to reduce IUC use and complication rates.