Background: Interdisciplinary rounding at the bedside is a recognized practice for improving patient care, communication, and teamwork. The Focused Interdisciplinary Team (FIT) Rounding model at UCSD has been in place since 2017. Since its implementation, our focus has been on sustaining the standardization of rounding practices and monitoring the impact of FIT on care quality and efficiency. The patient care information discussed during FIT rounds holds significant value for the workflow and care coordination of all rounding team members. Its potential utility could be extended more broadly to enhance the support provided during a patient’s hospitalization if incorporated into the Electronic Health Record (EHR).
Purpose: Our objective was to design and implement an EHR documentation tool facilitating real-time input of care plan elements, quality measures, and patient flow metrics during bedside interdisciplinary rounds. We aimed to create a tool that would make crucial data discussed during rounds promptly available to all care providers, track fidelity of our FIT rounding model, and help assess the impact of FIT on patient flow metrics and care quality.
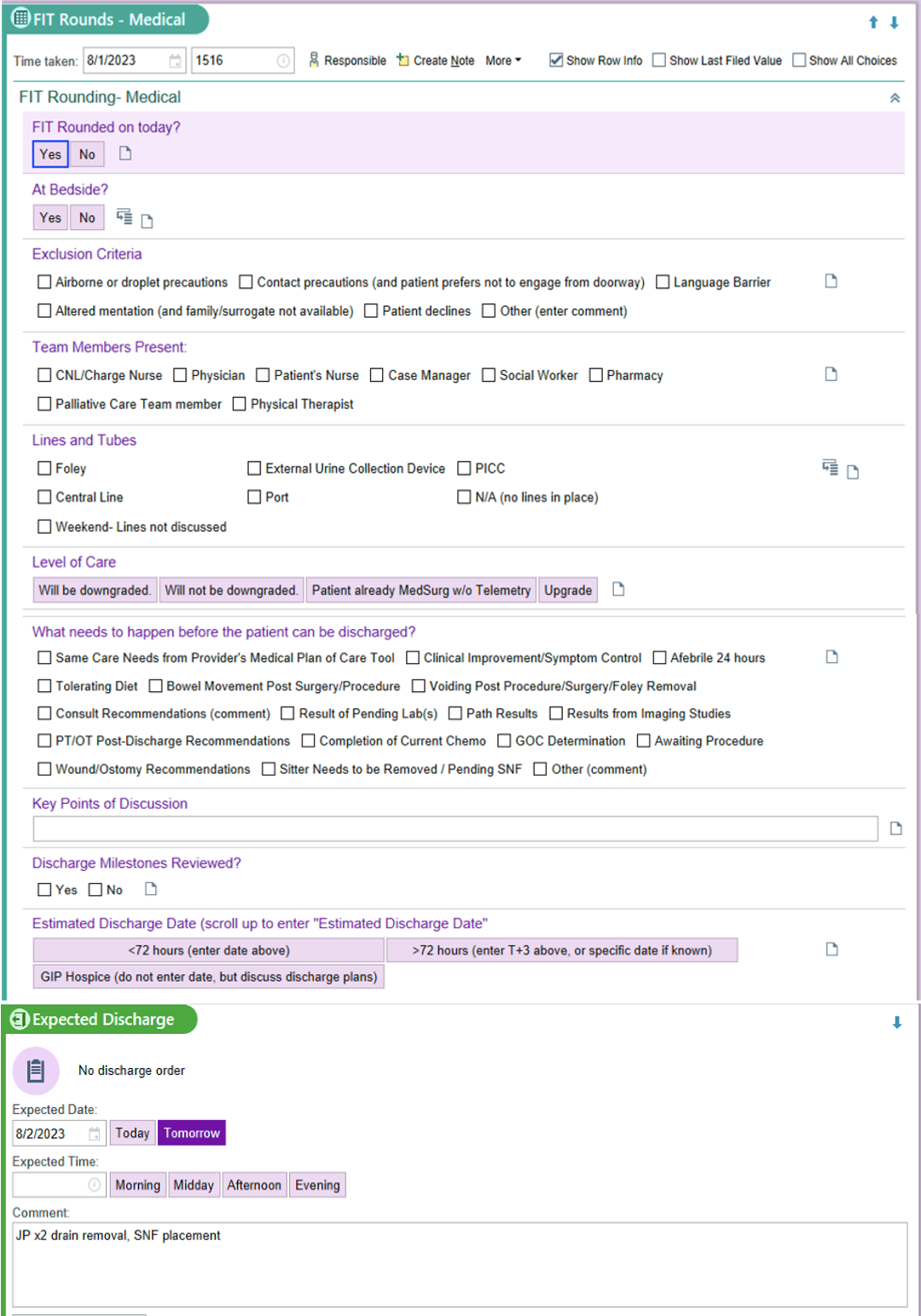
Description: We formed a multidisciplinary work group with representation from hospital medicine, nursing, information technology, and transformational healthcare to design an embedded EHR rounding tool. Leveraging our varied skill sets and perspectives, we created a simple navigator (figure 1) to input information shared during our interdisciplinary rounds. Via click boxes and drop-down lists, the user records information regarding FIT rounds fidelity (whether the patient received FIT, whether rounds occurred at bedside, which team members were present), invasive care de-escalation (lines/tubes present and justification), medical plan (clinical reasons for continued admission) and patient flow (level of care needs, non-clinical barriers to discharge and estimated date of discharge). We appointed the two clinical nurse leaders (CNLs) who lead FIT rounds to enter data into the navigator during rounds. The FIT Navigator was piloted for 5 months on two hospital medicine units comprised primarily of oncology/palliative care patients. Its use was trialed on both a laptop workstation on wheels and a handheld tablet. CNLs provided feedback that entry into the navigator on the laptop was easy and did not distract from clinical discussion or detract from their ability to lead rounds, while the tablet was not user-friendly. The documentation tool empowered nurse leaders to ensure that quality measures were discussed on each patient every day. Fidelity of the rounds was easily tracked remotely, allowing identification of opportunities for re-education and resource advocacy. This tool also provided opportunities for non-attendees to review discussion topics, aiding charge nurses in discharge planning and unit staffing. Over the course of the pilot, trends in improved patient flow metrics (including estimated date of discharge accuracy and average length of stay) were noted as well.
Conclusions: Implementation of an EHR documentation tool during bedside interdisciplinary rounds represents a step towards more streamlined patient care. By entering data in real time, we can ensure that vital information is promptly available to all care providers. It empowers rounds coordinators, promotes rounding fidelity, and can be a useful tool in evaluating the influence of multidisciplinary rounding on quality care metrics.