Background: The Intermediate Care Unit (IMU) was developed in the 1960s – 1970s as a level of care between general medicine (GMU) and intensive care units (ICU) [1]. The Society of Critical Care Medicine has established guidelines for admitting patients to an IMU based on severity of illness or need for frequent or complex nursing care [2].
Ensuring patients are consistently at an appropriate care level requires providers to perform ongoing assessments of patient clinical condition and care needs. Appropriate initial assignment to IMUs will likely reduce cost and improve patient flow. In 2017, UC San Diego Health hospitals added a requirement in IMU electronic medical record (EMR) admission and transfer order sets that required admitting physicians to electronically indicate why patients needed this level of care. Justification for level of care is only required at time of admission to the IMU; daily justification in the EMR is not required. This study compares appropriate IMU use before and after requirement of IMU justification in the EMR.
Methods: Charts of adult medical and surgical patients admitted to IMU level of care at two academic hospitals during two 14 day periods were retrospectively reviewed by a group of practitioners including hospital medicine physicians, a patient flow nursing supervisor and an internal medicine resident. The first review period was before justification of IMU level of care in the EMR was implemented. The second review period was after the requirement of justification. During both review periods, charts of patients at IMU level of care were evaluated to see if the patients met criteria for IMU level of care (Table 1).
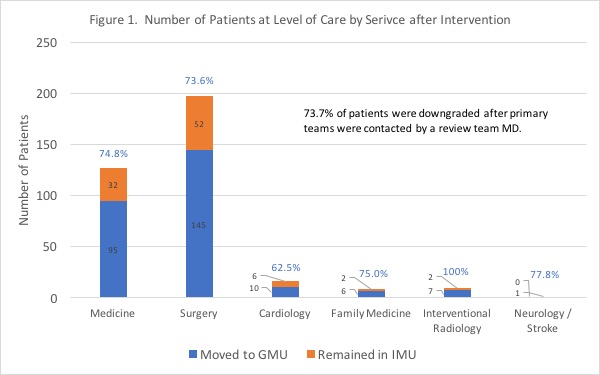
Results: For the 14-day period performed before justification of IMU level of care was required in the EMR, 688 of 1053 (65.3%) of patient-days were appropriately triaged to IMU level of care. Results for the chart review performed after implementation of required IMU justification are shown in Figure 1. During this period 988 of 1285 (76.9%) of patient-days met IMU level of care guidelines.
Conclusions: Effective interventions in EMR workflow can spur clinical quality improvement. Appropriate use of IMU beds and their associated intensive care could lead to both decreased patient-day costs as well as improved patient flow in and out of ICUs and emergency departments. Our study identified an EMR intervention that significantly increased the appropriate use of IMU level of care. Requiring justification of IMU level of care in physician admission and transfer workflow led to an 11.6% (65.3% to 76.9%) improvement in appropriate IMU use over the period studied. Earlier appropriate downgrade of patients to GMU level of care may also reduce admission cost although further work is needed to assess cost savings. This current intervention only requires providers to justify IMU level of care upon patient transfer to the IMU. Daily justification of IMU need may further improve these results but this should be implemented in a way to minimize additional work burden on hospital physicians. Improved communication between emergency department physicians, intensivists, hospital physicians, and surgeons would also likely improve appropriate IMU use. At academic hospitals, training house-staff in appropriate guidelines also proves an ongoing challenge. Finally, the effects of progressive care units, patient co-horting by location, and changes in physician workflow such as dividing care between admitting and rounding teams offer areas for further investigation.