Background: The ACGME has developed competencies for systems-based practice and problem-based learning and improvement to encourage trainees to integrate quality and safety into their everyday practice. Furthermore, the AAMC has a call to action for US Medical schools and teaching hospitals to successfully align clinical and education missions in order to have quality improvement and patient safety integrated into everyday practice. It is imperative that future physicians understand health systems science. In order to provide this learning opportunity, graduate medical education needs to work synergistically with healthcare delivery systems. There are many barriers to implementing strategies for this to occur, such as time limitations, resident and faculty commitment, and difficult-to-change institutional culture. Therefore, it can be difficult to teach residents about a large hospital system, their role within it, and how to make meaningful changes.
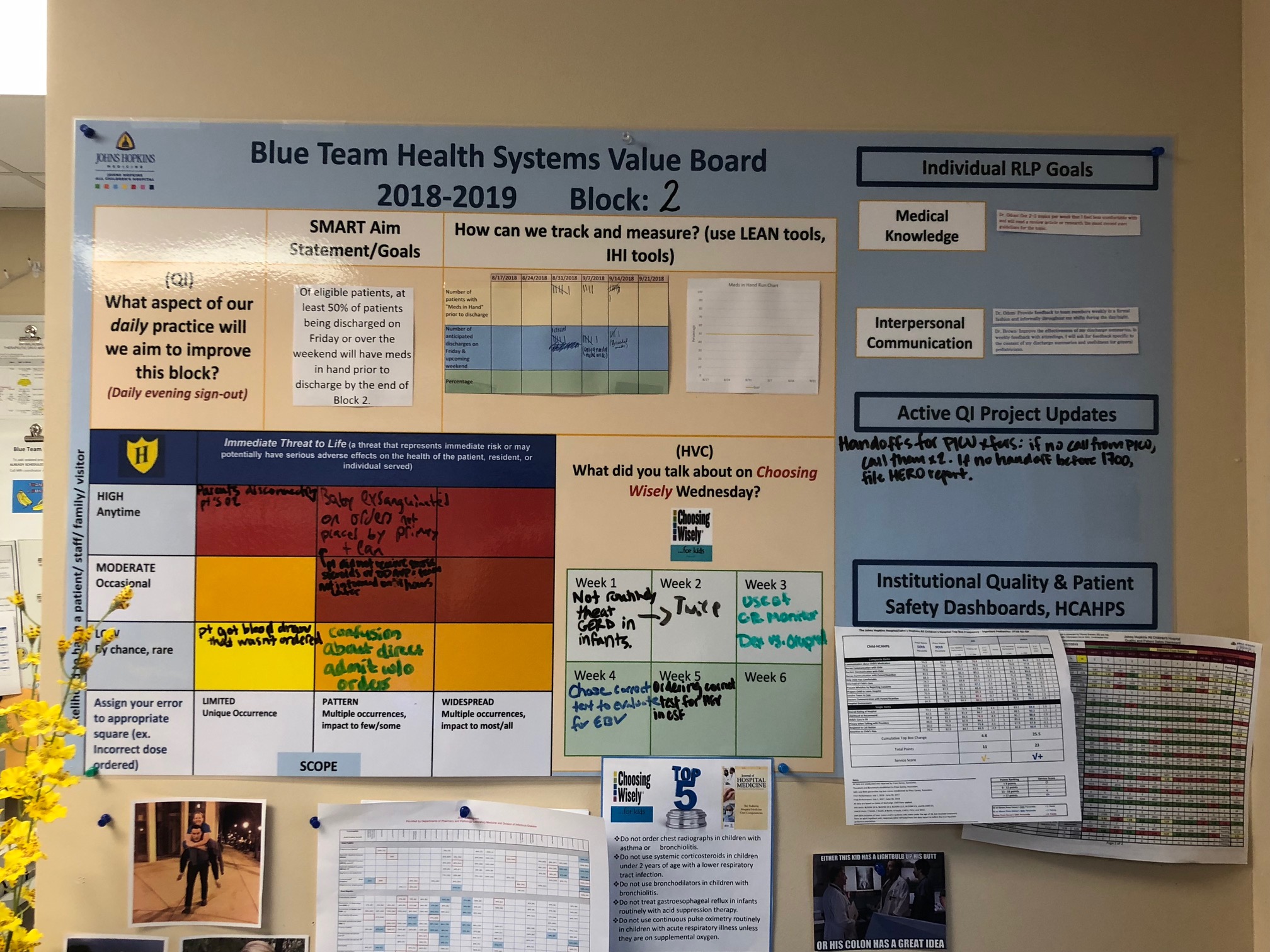
Purpose: We created the Health Systems Values Board to be utilized during the resident’s inpatient hospital medicine rotation. This dynamic board housed in the resident workroom allows resident teams to develop goals within a larger health care system to improve patient safety and quality. The board is resident-led with the goal to integrate into the culture of the inpatient service – to be as routine as patient handoff.
Description: The Health Systems Value Board is comprised of 6 sections to be referenced and completed throughout the inpatient wards rotation. The first section is dedicated to a team-lead quality improvement project, including an area for the team’s S.M.A.R.T. aim and space to track their progress through a run chart. The quality improvement project tracked in this section is selected by the senior resident class at the beginning of the academic year based on prior wards experiences.Another section of the board tracks incident reporting. In this section, residents are asked to stratify the events that occurred by harm or potential harm to the involved parties and the likelihood of recurrence. Themes reported from this area plan to be reported to the inpatient unit CUSP team quarterly.
Another section of the board is dedicated to tracking “Choosing Wisely” discussions, which encourages residents to engage at least once weekly in critically examining medical decisions made by the team to optimize high value care.
The next section is dedicated to residents’ individual goals for medical knowledge and interpersonal communication during the rotation to promote peer feedback and also illicit individual learning opportunities. Additionally, there is an area for ongoing resident-led inpatient QI project updates.. Our institutional safety dashboard and information on patient satisfaction surveys is housed in the last section..
Conclusions: The Health Systems Value Board is an initiative lead by the Johns Hopkins Pediatric Residency Program to allow better resident understanding of the larger hospital system and how to make meaningful changes within a health care system. Furthermore, it promotes quality improvement as a part of everyday medical practice, and stresses the importance of patient safety and quality, which addresses the call to action by the AAMC and ACGME. This board allows our program to increase exposure for the core pediatric milestones. While it has been fully implemented for twelve weeks, we have seen an increase in incident reports made by the wards team and completion of individual resident rotational learning plans in that time.