Background: Poor communication among providers is a barrier to seamless transitions in patient care. This problem is compounded when patients undergo interhospital transfer (IHT), where complex patients are transferred between providers, settings and healthcare systems. Templated notes have been used in other hospital-based care transitions to improve communication but have not been widely utilized during IHT.
Purpose: To develop and implement the use of an IHT “accept note” template for patients transferred from any outside hospital to general medical (GMS), cardiology, and oncology services at Brigham and Women’s Hospital (BWH), a 740-bed tertiary care referral hospital.
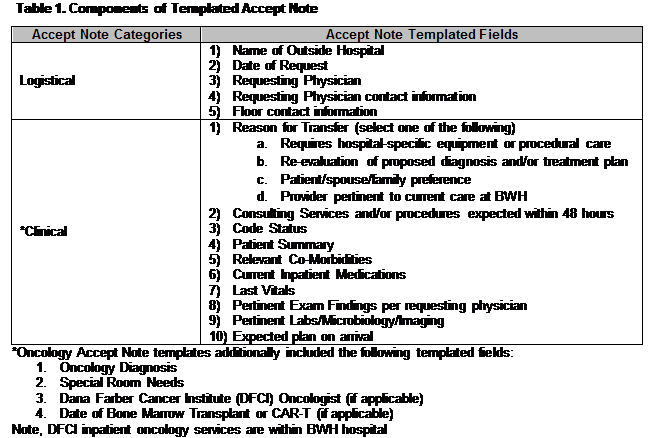
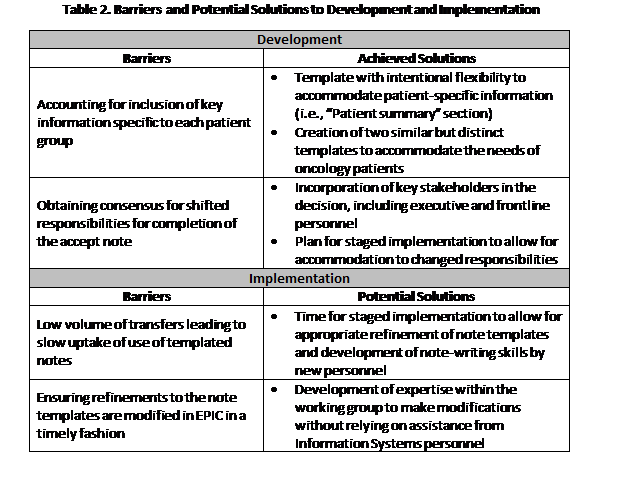
Description: Development of the templated accept note included input from key stakeholders, including leadership and frontline providers from the BWH Access Center and all included clinical services. Templates were designed, iteratively reviewed, and built into the hospital’s electronic health records, EPIC. Two templates were ultimately created: one for GMS and cardiology transfers, and one specific for oncology transfers given the specificity of information for this service (Table 1). Implementation of the accept note templates is occurring in a step-wise fashion: for all GMS transfers on 11/3/18, and for nighttime/weekend cardiology transfers on 11/17/18, with planned expansion to all cardiology transfers and all oncology transfers by the middle of December. Responsibility for completing the accept note was shifted from the accepting clinician to Access Center nurses at time of implementation. We are evaluating the availability and quality of accept notes over time, using retrospective chart review to determine their presence and inclusion of key data elements. Frontline physicians are also surveyed biweekly on their perception of availability and quality of accept notes and how this has impacted their care of transferred patients. We have identified several barriers and potential solutions to development and implementation (Table 2).
Conclusions: We have successfully designed and initiated implementation of templated accept notes for use during IHT to medical services at a large tertiary care hospital. Our goal is to improve essential communication and clinical data exchange to ultimately improve the quality and safety of IHT. Though we have encountered described barriers to implementation, we anticipate successful implementation, ongoing refinement, and future dissemination of our intervention, which will be guided by ongoing stakeholder input and measurement of its impact on the quality and safety of transferred patients.