Background: Cardiac monitoring (CM) is often overused, hindering patient mobility, triggering unnecessary cardiac testing, delaying appropriate discharge, and expending resources.
Purpose: To reduce the days that medical and surgical ward patients spend on CM without an indication specified in the 2004 American Heart Association (AHA) guidelines for CM.
Description:
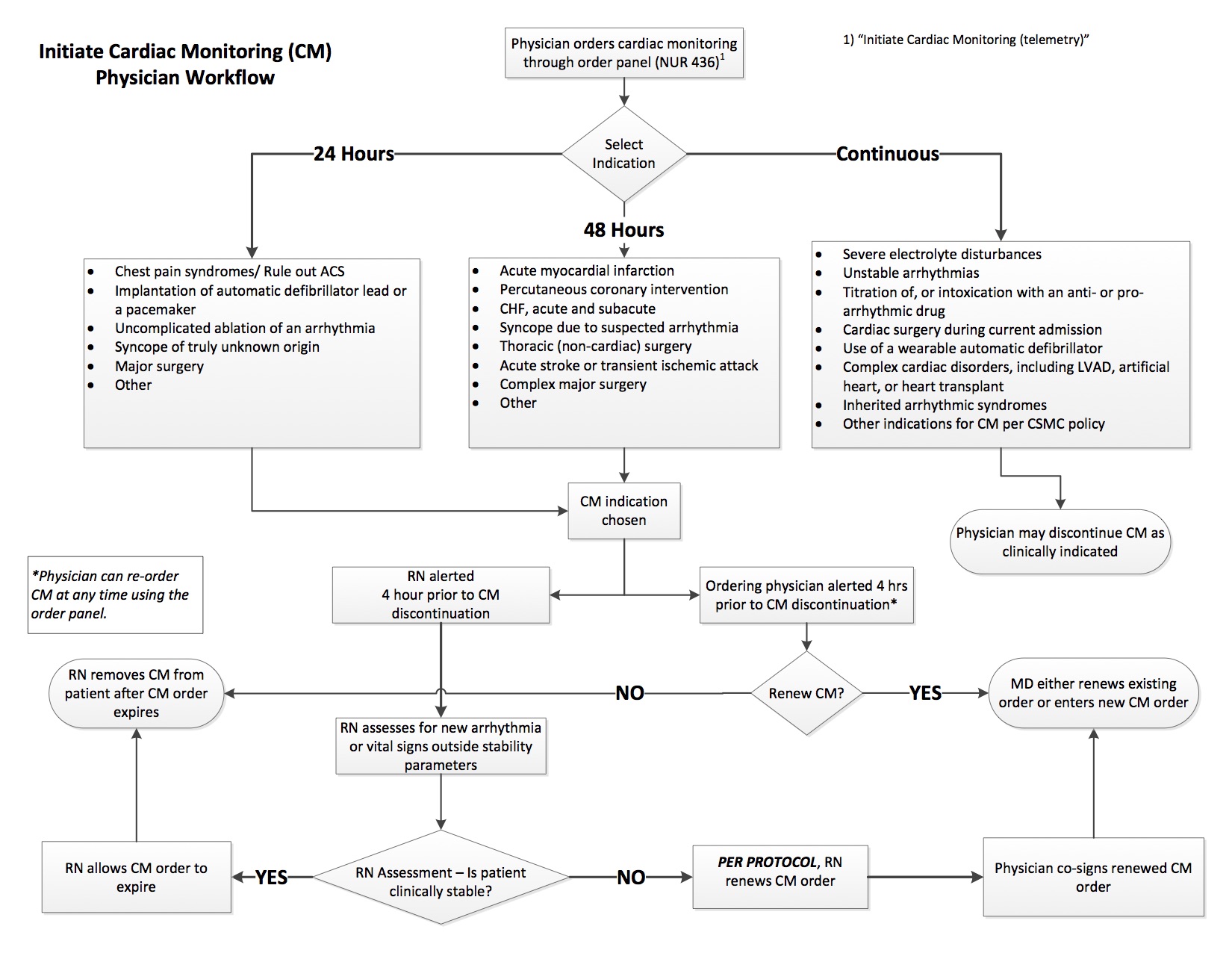
At Cedars-Sinai, only 59% of patients on CM had an AHA-approved indication for CM. Physicians were able to order CM without specifying an indication or stop date, and could keep patients on CM indefinitely. Prior efforts to reduce unnecessary CM use, including academic detailing, had not been effective. Using our electronic medical record, Epic™, we implemented a modified version of the AHA guidelines throughout the all adult medical-surgical units. Providers now prescribe CM by selecting a clinical indication, as they would for any diagnostic test. Each clinical indication has an associated duration—24 hours, 48 hours, or until the provider stops the CM (Figure 1). With time-limited indications for CM, four hours prior to the assigned expiration, both the ordering physician and bedside nurse receive an alert. Physicians have the option to renew the CM, discontinue the CM, or defer to another provider. Nurses are offered similar options, as well as instructions to assess clinical stability. If the patient has unstable vital signs or a new or worsening arrhythmia, the nurse can renew the CM. Although a physician’s response to the alert trumps the nurse’s response, if the patient is stable and the physician has not reordered the CM, the nurse can discontinue it. Nurses may also defer to the patient’s primary nurse.
To date, physicians have received 403 alerts on 143 patients and nurses have received 1657 alerts on 185 patients that time-limited CM orders were expiring. No alerts resulted in a physician or nurse continuing the CM. Physicians discontinued the CM after 58 alerts (14.4%), deferred to the primary physician on 72 alerts (17.9%), and exited 273 alerts (67.7%) without a response. Nurses discontinued the CM after 71 alerts (4.3%), deferred to the primary nurse on 10 alerts (0.6%), and exited 1576 alerts (95.1%) without a response. In total, this process ensured that CM was time-limited on 129 of 331 patients (40.0%). Neither physicians nor nurses have voiced concerns about effects on patient safety or a time burden associated with responding to the alerts. Collection of data on reasons for CM, total number of patients on CM, total time patients spend on CM, and safety related to time-limited CM (e.g., codes blue, rapid responses) is ongoing. Further investigation of reasons for exiting the alert without action is needed.
Conclusions: Based on data obtained to date, using a clinical decision support intervention to implement the AHA guidelines on CM has been acceptable to physicians and nurses, and has triggered clinically appropriate discontinuations of CM, in accordance with the 2004 AHA guidelines.