Background:
Transfusion of red hlnnri cells (RBCs) in the appropriate clinical setting can be a lifesaving procedure, but This therapeutic power does not come without cost. The latter cannot only be measured in dollars, but also in risk of harm to the recipients. Recent data suggest that blood transfusions are independently associated with increased nosocomial infection rates, cancer recurrence rates, anc even increased mortality. The critical judgment that faces clinicians, therefore, is the determination of the severity of anemia [as measurec by serum hemoglobin (Hgb)] at which the benefit of a blood transfusion outweighs the risk in a particular patient. Unfortunately, current national guidelines, which are heavily reliant on expert opinion, are intentionally vague on recommended practices for patients wilh Hgb belween6and 10 g/dL. As a result, inappropriate transfusions occur. Furthermore, data from randomized trials indicate lhat patients tolerate, and even tend to fare better, when managed with a restrictive transfusion strategy (treat if Hgb < 7) versus a liberal transfusion strategy (treat if Hgb < 9), Given The potential for improved outcomes and lower cost, more judicious use of RBCs directed by more specific data‐driven guidelines should be encouraged.
Purpose:
To develop and implement an evidence‐based institutional guideline, computerized physician order entry alert, and feedback mechanism to assist clinicians in their determination of when To treat anemic patients with RBC transfusions.
Description:
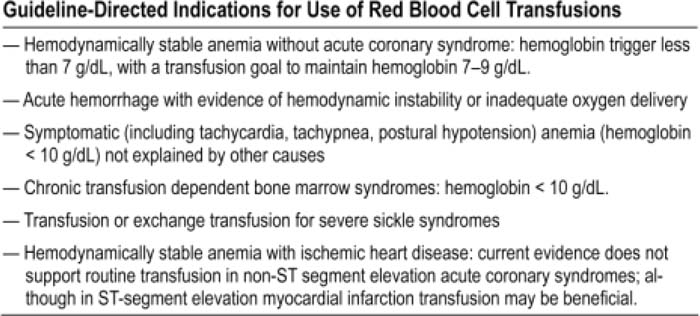
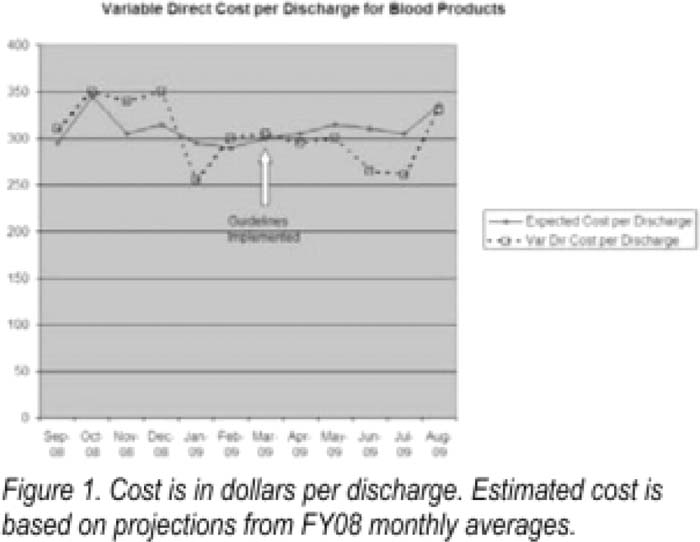
Analysis of the use of RBC at the University of Michigan Hospital revealed that The cosT had risen from 311 million in FY04 to $15 million in FY0G. apparently driven by increased use per patient. Remarkably, 47% of hospital admissions were transfused with some type of blood product in FY08. In response, a multidisciplinary committee was formed to generate and evaluate possible solutions To reduce inappropriate use of RBCs To both reduce cost and to improve patient outcomes. A Lean analysis of the transfusion procedure indicated lhat the majority of waste in the system stemmed from clinicians ordering blood products in potentially inappropriate clinical situations. Institutional guidelines were developed and approved. A mullimodal strategy was implemented including: education of clinicians via lectures on the newer, more restrictive transfusion strategy, delineation of risks associated with transfusion, and use of computer‐generated alerts on the inpatient order entry system when a RBC transfusion was ordered for patients with a Hgb > 7 or no recent Hgb. Finally, reports for monitoring blood product use by individual physicians and departments were developed. Preliminary data (see Fig. 1) indicate that implementation of this strategy has resulted in a trend toward decreased cost and use of RBCs.
Conclusions:
Rapid implementation of RBC guidelines at major teaching hospitals can be achieved and will likely result in more appropriate use.
Author Disclosure:
J, Rohde, University of Michigan, employment; T. Laing, University of Michigan, employment.