Background: Hospital readmission rates are heavily scrutinized, and are utilized as a measure of the quality of care provided by hospitals. In the Oklahoma City Veterans Affair Health Care System (VAHCS), there was a significant increase in the number of cardiorespiratory 30-day readmissions in the month of September (8% to 14%). Most patients (76%) were readmitted within 14 days. We aimed to decrease 14-day cardiorespiratory readmissions by 6% in 3 months.
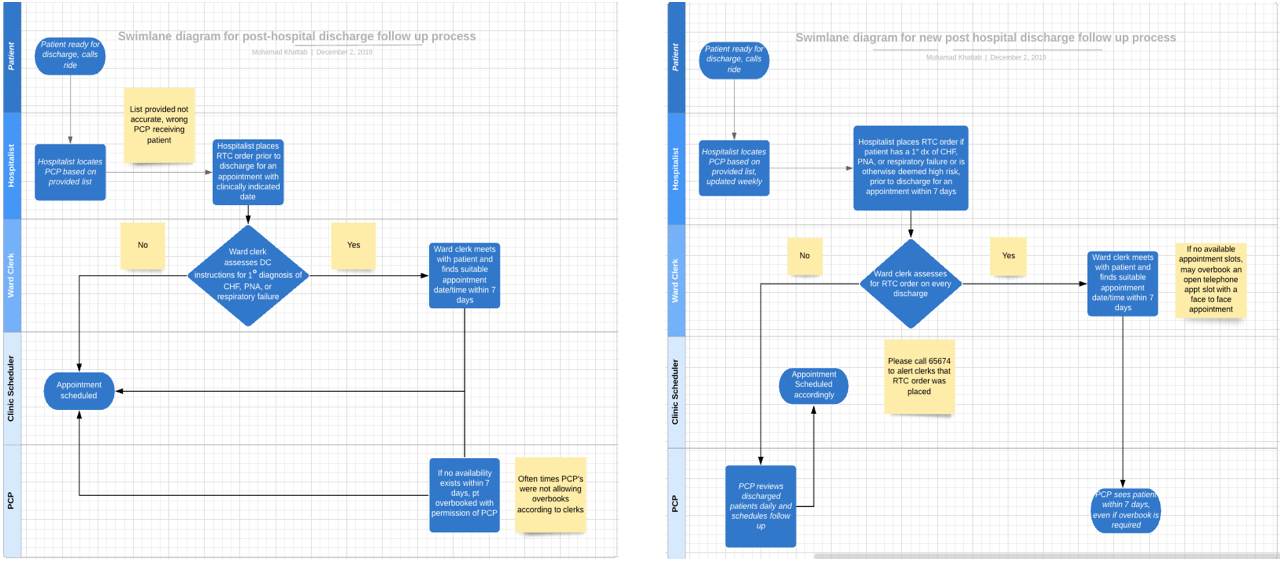
Methods: Data regarding total number of cardiorespiratory discharges and readmissions was obtained via the VA corporate data warehouse, and our team confirmed accuracy of data via chart review. Cardiorespiratory was defined as patients with a primary discharge diagnosis of: heart failure, pneumonia, or respiratory failure. Our outcome measure was 14-day cardiorespiratory readmission rate, and process measures were follow-up rate in primary care clinic within 7 days, and number of transfers incorrectly coded as readmissions. Data was plotted on a run chart and the Westgard rules for interpretation were used to assess for nonrandom variation. We noted that 13% of cardiorespiratory readmissions were in fact patients who were transferred to another facility for a procedure, and upon return, were coded as readmissions. We also noted that most patients (64%) who were truly readmissions were readmitted between 7 and 14 days. Plan-Do-Study-Act (PDSA) 1 occurred over 20 days, and included a formal didactic to ward administration staff regarding appropriate coding of patients returning to our facility after transfer. PDSA 2 occurred over 15 days and included redesigning our discharge process by asking hospitalist teams to ensure 7-day follow up in primary care for all cardiorespiratory discharges (see figure 1). PDSA 3 occurred over 15 days and involved improving the intervention in PDSA 1. We noted that while education occurred for some staff, due to high staff turnover not all employees were aware of this new process change. We provided a flow chart describing the transfer process, made it available on all floors, and included education on this process in orientation for all new employees.
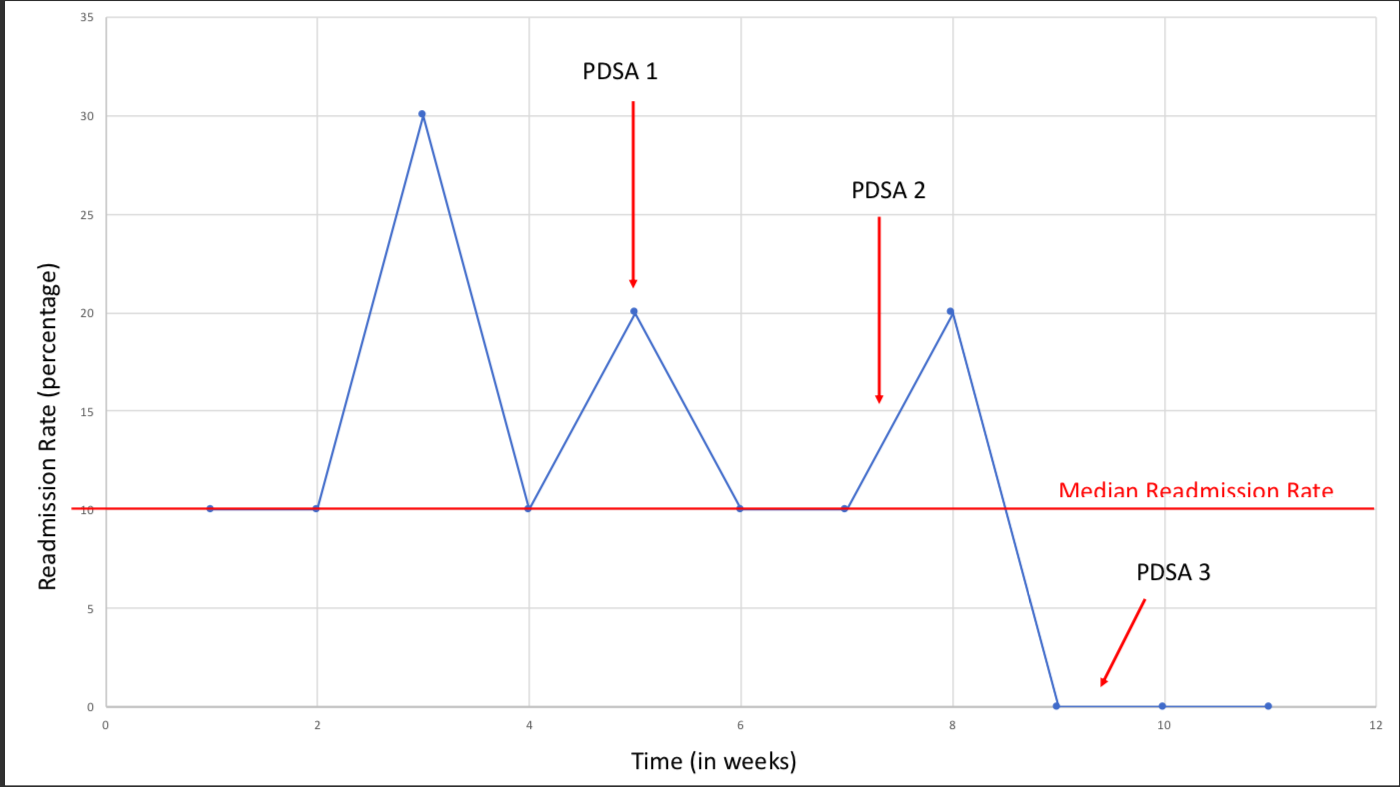
Results: A total of 110 patients were assessed over 11 weeks. A total of 12 patients required readmission within 14 days of discharge. Patients were assessed sequentially based on time, in order to assess the impact of our interventions as they were instituted; however, we grouped them into groups of 10 for a more uniform denominator. The 7-day primary care follow-up rate increased from 14.3% to 71.4% after PDSA 2. The number of transfers incorrectly coded as readmissions decreased from 10% to 0% after PDSA 3. Readmission rate varied between 10-30%, decreased to 0% after PDSA 2 and remained 0% for another 1.5 weeks after PDSA 3 (see figure 2). With a median readmission rate of 10%, 11 data points and only 1 run, we feel confident that this represents a nonrandom change.
Conclusions: Cardiorespiratory readmission rates were high in September, but have since decreased significantly. Our project highlights the significance of close monitoring after interventions are instituted to adjust and improve chances of success, as noted with PDSA 3 after PDSA 1 was unsuccessful. Proper coding of transfers and redesigning the discharge follow up process to ensure 7-day follow up helped significantly decrease cardiorespiratory readmission rates. Long term follow up is required to ensure sustainability of these results.