Background: Acquired hyponatremia and hypernatremia are common in hospitalized patients and correcting dysnatremia may improve outcomes. Nephrology assistance with dysnatremia may help optimize management, but specialist resources are limited. Targeted Automatic e-Consultation (TACo), a model of selective e-consultation based on automated identification of patients from the electronic health record, has been applied for glycemic management in hospitalized patients. Dysnatremia may be another potential target for TACo, particularly if there is under recognition or mismanagement of dysnatremia. Our study assessed the prevalence of inpatient nephrology consultation for dysnatremia and surveyed hospital medicine physicians’ perception of the utility of TACo for dysnatremia.
Methods: This study was conducted in two phases. We first conducted a retrospective analysis of all adults hospitalized in FY18 at a large academic medical center, identifying encounters with persistent (3 or more consecutively abnormal serum sodium values) in-hospital hyponatremia or hypernatremia that was not present on admission. We excluded patients on hemodialysis or comfort-care, patients on the obstetrics and gynecology service, and patients on the neurosurgery service (for hypernatremia only). For each encounter, we assessed variables including primary service, severity and duration of the dysnatremia, whether it was resolved at discharge, and whether nephrology was consulted. These were reported as medians with interquartile ranges. P values were calculated using the Chi-Square test on a 2×2 table. In the second phase, we electronically surveyed hospitalist attendings and residents regarding their perceptions of receiving targeted advice through the TACo model using a modified Likert scale.
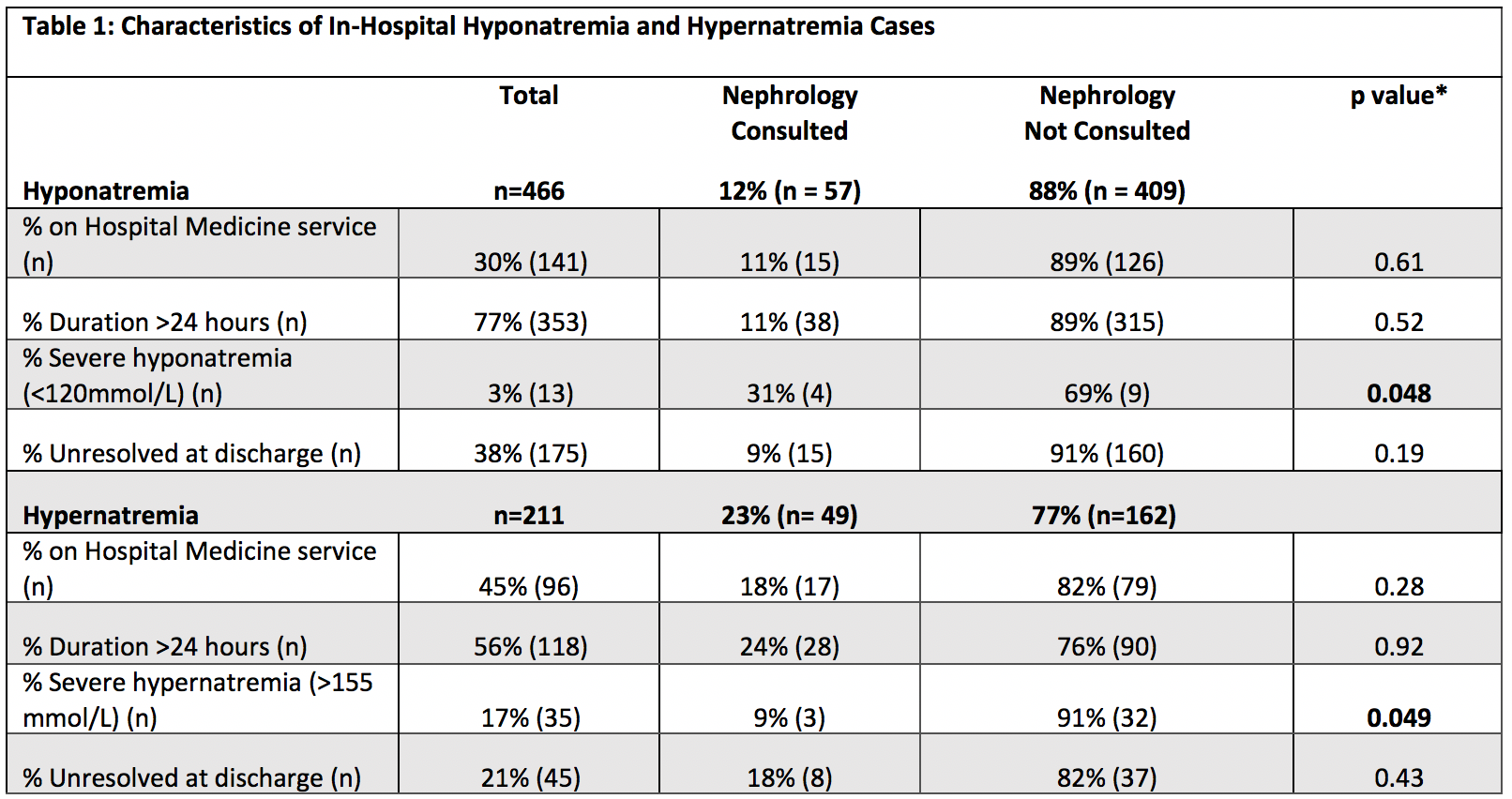
Results: Of the 6889 discharges in FY18, 466 cases of in-hospital hyponatremia and 211 cases of in-hospital hypernatremia met inclusion criteria, accounting for (6.8%) and (3.1%) of total discharges, respectively. The median duration of hyponatremia was 37.6 hours (IQR 18.0-67.6) and of hypernatremia was 35.3 hours (IQR 13.9-70.9). A total of 3% (13/466) of hyponatremia cases were severe (sodium 155mmol/L). Nephrology was consulted in a minority of severe cases of both hyponatremia (31%) and hypernatremia (9%) (Table 1). Of 102 surveyed physicians, 59 (58%) completed the survey and 68% (40/59) responded that a hyponatremia TACo would be either “very useful” or “useful.” For hypernatremia, 51% (30/59) reported a TACo would be either “very useful” or “useful.”
Conclusions: Nephrology was consulted in only a minority of hyponatremia and hypernatremia cases in this large, urban academic medical center, even when the sodium abnormality was severe. Patients were often discharged with unresolved hyponatremia or hypernatremia, suggesting an opportunity for improved management. Most internal medicine survey respondents thought a TACo for in-hospital dysnatremia would be useful. Based on these data, we conclude that targeted automatic e-consultation may be a useful strategy to improve management of in-hospital dysnatremias.