Background: Patients with advanced cancer have high readmission rates, up to 27% in some studies, and represent unique challenges related to transitions of care, complex disease management, and care coordination. Recent efforts have focused on better identification of potentially avoidable readmissions (PARs). One study found that primary reasons for PARs in cancer patients included pre-mature hospital discharge and lack of timely follow-up, and that patients with higher symptom burden were more likely to experience PARs. While there is increased evidence to suggest reasons for PARs, there is no gold standard on an optimal approach to addressing and preventing these issues.
Purpose: The Clinical Assessment and Rapid Evaluation (CARE) Clinic is an innovative urgent care facility focused on reducing unnecessary emergency department (ED) visits and hospital readmissions for oncology patients by providing treatment for urgent medical and symptom-related issues, improving transitions of care, and early identification and intervention for patients at increased risk for readmission.
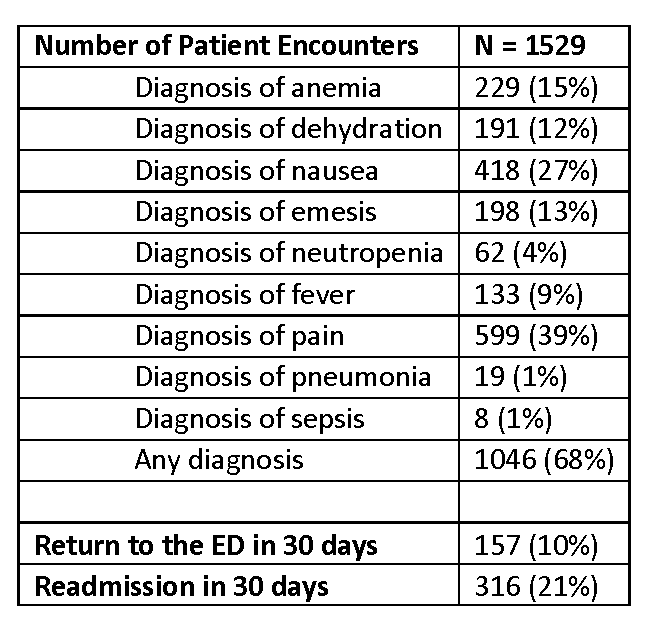
Description: The CARE Clinic is a collaborative effort between the Division of Hospital Medicine and the Division of Oncology and is staffed jointly by Advanced Practice Providers (APPs) in both divisions. Hospitalist APPs in the CARE Clinic also work on the inpatient Oncology Hospitalist service and have significant experience in complex symptom management frequently seen in cancer patients, while Oncology APPs have advanced knowledge in individual chemotherapy/immunotherapy regimens. By bridging these roles, patient in CARE are able to receive urgent care services from a team of providers with specific knowledge related to their disease process, ensuring patient-centered care. CARE provides a variety of diagnostic and treatment services including IV fluids, anti-emetics, pain medications, and antibiotics, as well as full laboratory evaluation and advanced imaging. Approximately 70% of patients seen in CARE in AY ’19 had visit diagnoses identified as ‘avoidable readmissions,’ with pain and nausea as the leading reasons for visits. In addition to these services, CARE also takes a proactive approach to reducing hospital utilization through early identification and outreach to patients identified as moderate to high-risk for readmission, and by providing close follow-up upon discharge from the hospital (within 24-48 hrs), which patients often are unable to obtain in primary oncology clinics. There is current work underway to create a shared inpatient/outpatient dashboard between CARE and the Oncology Hospitalist service, to identify areas for early intervention. APPs in the CARE clinic communicate regularly with patients’ primary oncology teams and inpatient hospitalist teams, working in a supportive and collaborative fashion. This model is the first of its kind and represents a unique opportunity for APPs to work at the top of scope, optimize resource utilization, and most importantly, improve the way that care is delivered to oncology patients.
Conclusions: The CARE Clinic represents a unique, innovative partnership between Hospital Medicine and Oncology, is a model of collaborative, top of scope practice for APPs, and improves the way that patients with cancer receive care. Continued studies are needed to identify the impact of discharge pathways and early identification/outreach on ED/hospital utilization, and to optimize the CARE model.