Background: Early discharge from the hospital improves hospital throughput as well as patient and staff satisfaction. At times, our emergency room tends to board many admitted patients for more than 24 hours, which further distresses our patients and staff. We noticed that the total number of patients leaving the hospital earlier in the day decreased in the last few years. By recognizing barriers to early discharges, we attempted to improve the total number of patients being discharged between 7AM and 2PM .
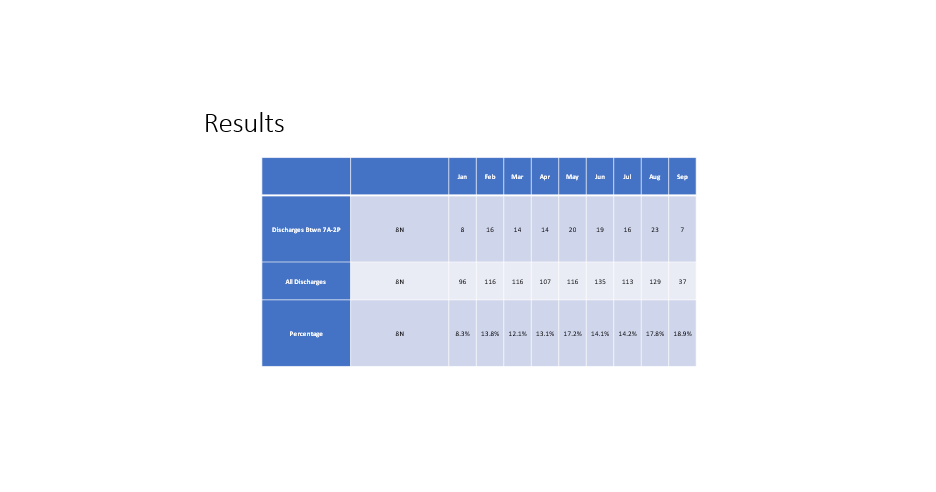
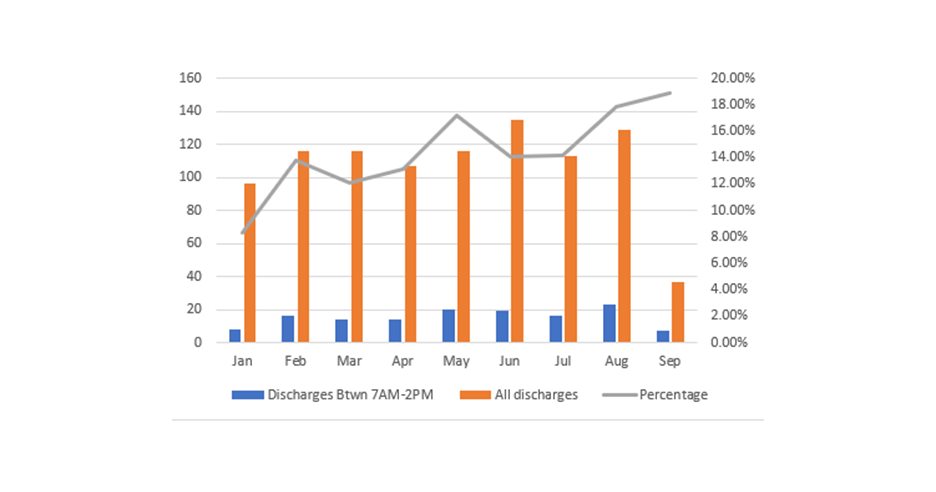
Purpose: This project targeted patient population on 8 North(8N), a medical hematology-oncology floor at our urban tertiary academic medical center. In 2021, the percentage of patients discharged between 7AM and 2PM was 13%. This rate worsened in January 2022 to 8.3%. A further look-back revealed that in 2019 the percentage of our early discharges was 18.7%. This consecutive sharp decline prompted an initiative to increase early discharges. With early recognition of potential discharge barriers, we aimed to increase the number of early discharges by implementing a discharge information tent card. The changes were implemented by March 2022 and data collected over next six months.
Description: We created an interdisciplinary discharge process centered around the utilization of a discharge tent card. The initiative was led by a hospitalist lead in conjunction with nursing, case management and social work. During our daily interdisciplinary rounds, we identified patients leaving within the next 24-48 hours. Our typical cohort of patients included: 1. Patients that were finishing radiation treatments 2. Patients that need long term IV antibiotics 3. Patients that were finishing inpatient chemotherapy regiment4. INR bridging There was a defined responsibility for each of our team members as follows: Case managers arranged transportation and home care -Social workers arranged early transportation to rehab -Nurses completed education around finger stick check, Insulin administration and Lovenox injections -Physicians and advance care providers communicated with patient and family about medications and follow appointments on discharge. medications were sent to the pharmacy the day before anticipated discharge to ensure medication was covered -As a team, we also assessed whether COVID testing was up to dateThe discharge tent card was given to the identified patients, prominently displayed in patient’s room 24 to 48 hours before discharge. This card maximized our collaborative efforts, and served as visual tool to alert our patients and family members of an early next day discharge. Metrics were obtained from our Information technology department that keep an active log of when patients are discharged from the floors.
Conclusions: After 6 months of implementing the discharge cards, we found an increase in the percent of discharged patients per month from 8.3% in January to 18.3 % in September with sustained improved discharge numbers before 2 pm consistently. Utilization of the discharge tent card has been an effective intervention to improve our early discharges. This intervention has enhanced patient centered communication and proved to be a cost-effective approach for discharge planning. The success of our unit’s initiative was noted and as a result our executive leadership team is looking to expand this initiative across the hospital.