Background: Baystate Children’s Hospital serves a population that is vulnerable to unsafe sleep practices. By July 2017, there were 6 cases of accidental infant deaths in Hampden County MA, attributed to unsafe sleeping practices, primarily due to co-sleeping. In Springfield, MA, infant mortality rate (9.2%) is double that of the state rate (4.4%). Rates of teen pregnancy, smoking during pregnancy, inadequate prenatal care, prematurity, low birth weight are all significantly higher in Springfield, MA than the state average. These health factors may correlate either directly or indirectly to increased cases of SIDS according to recent research. As Baystate Medical Center is the largest hospital system in Springfield, MA, a hospital-based intervention focusing on Safe Sleep could decrease the high rate of co-sleeping and other dangerous safe sleep practices during the hospital admission.
Purpose: The overall aim of this project is to improve the percentage of infants in safe sleep positioning (SSP) on the Inpatient Pediatric Ward at Baystate Children’s Hospital to 90% through quality improvement (QI) methods. This will be accomplished primarily through parent education, role modeling proper SSP, and also adding components of staff education (nurses, PCTs, residents, attendings). Our hypothesis is that by improving education surrounding safe sleep positioning in the Baystate Children’s Hospital pediatric ward primarily through parent education and role-modeling proper safe sleep positioning will improve rates of SSP on the pediatric wards, determined by night time audits, to 90%.
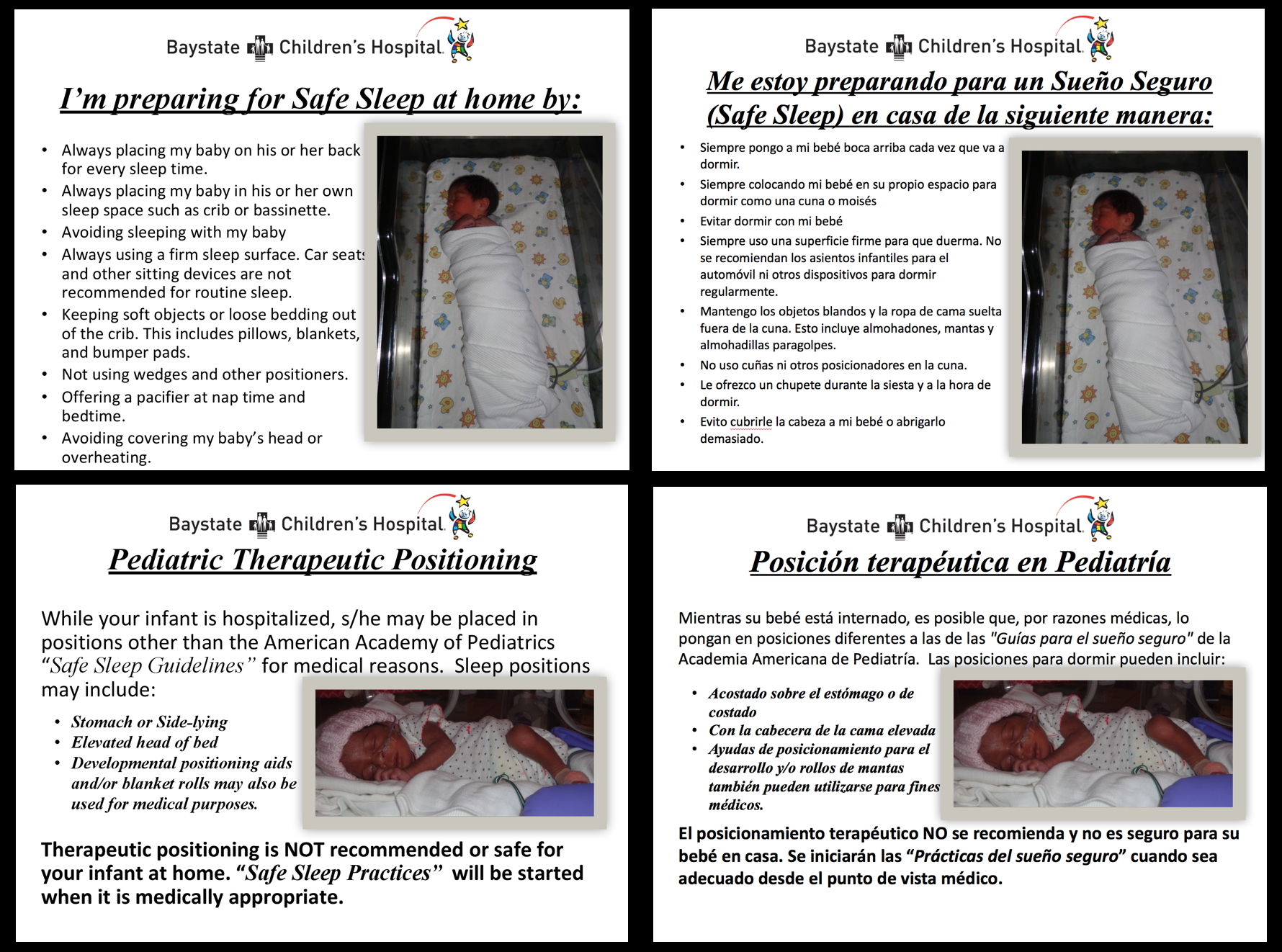
Description: This is a QI study, with baseline data being collected over a period of 2 weeks by the night team residents on the floor. On night rounds, between 10PM – 12AM, they will observe the sleeping positions of all patients ages 0 – 12 months of age and will document their observations. Documentation will include a checklist describing the observed sleeping position and situation. Data will be entered into Tufts CTSI REDCap, a secure electronic database. The first PDSA cycle will focus on caregiver education, in the form of a card placed at the bedside with a picture of an infant in SSP and an explanation of SSP. Cards will be available in both Spanish and English and will be cards that have been adapted from the ones currently used in the Baystate Children’s Hospital NICU. If the infant is has not been placed in safe sleep purposefully for therapeutic reasons, there will also be a card indicating that the infant is in “therapeutic sleep positioning,” along with the card showing SSP. The second PDSA cycle will also be focused on patient/parent education. On admission to the inpatient floor, parents will be given the AAP handout on safe sleep by their nurse or by the admitting resident. Parents will be informed that we promote safe sleep positioning in our hospital and will be asked to read the handout. The third PDSA cycle will focus on patient education through the use of Family Centered Rounds (FCR). The day inpatient resident teams and attendings will receive a script to follow to discuss safe sleep on FCR and the first time they round on a newly admitted infant.
Conclusions: Improving SSP in the inpatient setting through QI methodology is a necessary component of a community-based strategy to improve SSP. Implementing an educational strategy that involves caregiver education with bedside cards, AAP educational materials, and reinforcement of SSP during FCR is feasible.