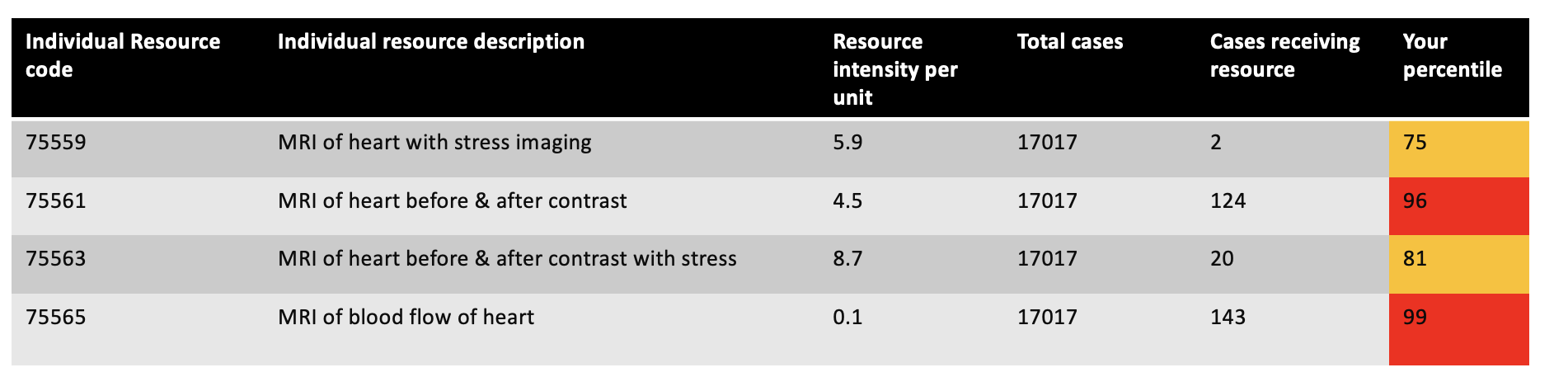
Background: Inpatient stewardship has appropriately become a large focus of acute inpatient care. The Vizient™ Clinical Data Base contains hospital discharge data used for benchmarking, and we observed significantly elevated cardiac MRI (cMRI) use at our tertiary hospital, relative to other tertiary academic medical centers, with resource utilization percentile averaging in the top decile (figure 1).
Methods: In an effort to better steward our limited acute care resources, we implemented an intervention to decrease use of cMRI that could more appropriately be done in the ambulatory setting. A multidisciplinary team consisting of cardiology, radiology and hospitalists was assembled, with leadership from Chief Medical Officer (CMO). Three intervention steps were taken. First was the development of agreed-upon criteria for inpatient cMRI. Evidence-based inpatient cMRI criteria included the following: 1. Evaluation of infiltrative cardiomyopathy in the setting of complete heart block of ventricular tachycardia, 2. Evaluation of acute myocarditis, 3. Viability evaluation prior to planned urgent revascularization (2). Second was implementation of radiology as a gatekeeper for inpatient imaging – if inpatient cMRI was ordered, but the patients did not meet the above criteria, radiology would reach out to the team to discuss indications. Third was the launch of concierge scheduling to expedite outpatient cMRI, with the goal of scheduling within 2 weeks post discharge. We used data from Vizient to track pre and post intervention cMRI use and compared length of stay (LOS) between patients who did and did not have cMRI within the same diagnosis-related group (DRG). We used this difference to estimate the hospital’s savings from the intervention at the admission level and projected this out for the year.
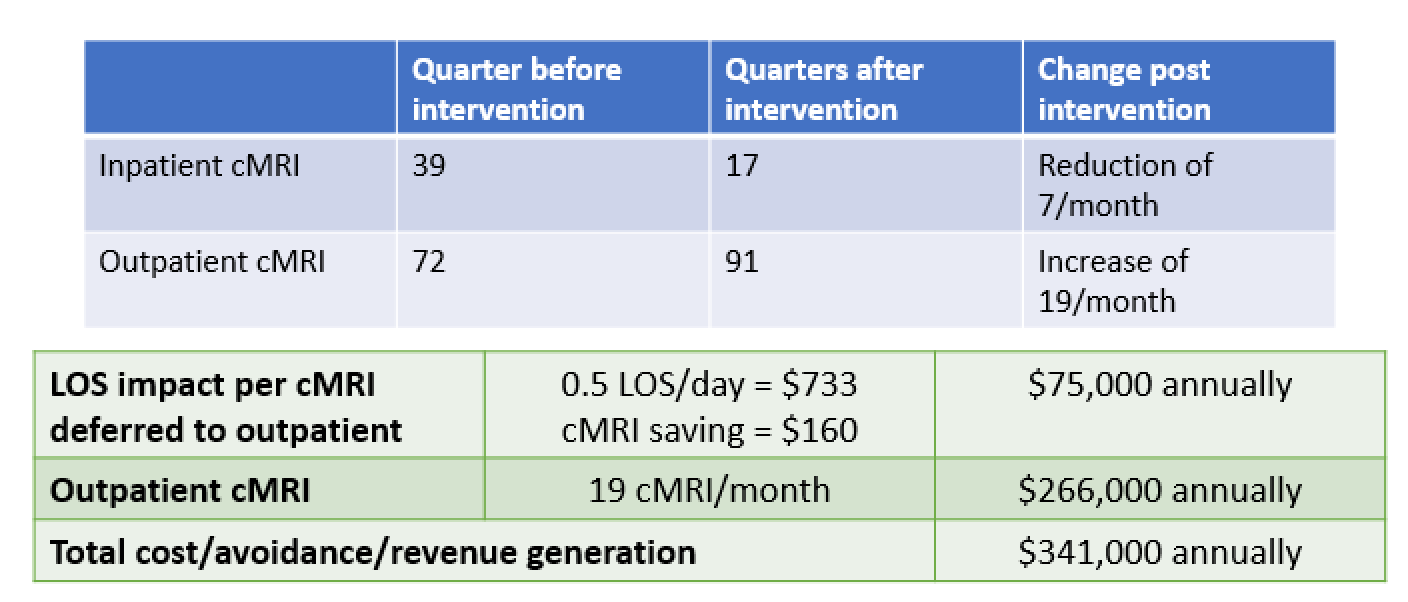
Results: Prior to the intervention, the average inpatient cMRI ordered quarterly was 39 (13 cMRI/month). After the intervention, the quarterly inpatient cMRI usage was 17, all of which met inpatient intervention criteria above. This is an average reduction of 7 cMRI/month. Additionally, we saw an increase of outpatient cMRI with an average of about 19 cMRI/month. Based on our internal data metrics and financial data (averaged across all payers), LOS was reduced by 0.5 day per patient for which cMRI was ordered as an outpatient (average cost of $733). The inpatient cost saving per cMRI not completed in-house was $893. Combined this translates to $75,000/year saved. Additionally, with the increase in outpatient scans, the total additional revenue generated by outpatient cMRI was $266,000/year. The total financial impact of this project (including cost avoidance and revenue generating) is $341,000/year.
Conclusions: Appropriate inpatient stewardship is essential for hospital throughput and for appropriate reimbursement with DRG payments. Via a multidisciplinary team approach, and creating clear guidelines for cMRI orders, our institution was able to reduce inpatient cMRI. Additionally, with improved outpatient access and radiology partnership, we reduced LOS by 0.5 days, increased outpatient cMRI, resulting in a total estimated project revenue generation of $341,000 annually.