Background: The American Board of Internal Medicine (ABIM) Foundation developed the Choosing Wisely project in 2012 as a way to identify commonly used tests that may be overused or inappropriately used. The Society of Hospital Medicine created a subcommittee in this project focused on recommendations affecting hospitalists, and made the recommendation in 2013 to stop repetitive complete blood count (CBC) and chemistry testing in clinically stable patients (1). An offshoot of this project was developed at MUSC, where the electronic health record (EHR) was used to reveal over-utilization of lab ordering. The analysis was performed at the attending level and distributed monthly. It initially reduced over-ordering of common blood work, but progress slowed and eventually reversed over time. Despite a loss of momentum in the campaign, over-utilization of labs still leads to deleterious effects such as hospital-induced anemia (2). Moreover, staff shortages have led hospitals to find innovative means to reduce workload and improve efficiency to maintain quality. Each year, the residents across graduate medical education (GME) at the Medical University of South Carolina (MUSC) organize a quality improvement (QI) project in their area. With EHR-generated reports, we looked at the existing data in a new way, at the level of service team. This small change in data analysis allows us to intervene at the level of the ordering provider–the residents.
Purpose: We aim to reduce CBC and chemistry testing on the resident-run ward teams over a 9-month period. The internal medicine residents organize and implement a QI project that relates directly to their work, while simultaneously taking a step toward solving a universal hospital problem. Additionally, this allows residents to make interventions in a controlled population and directly observe the effect of the intervention. Finally, this has hospital-level effects by reducing costs, decreasing nursing and phlebotomy workload, and improving patient satisfaction.
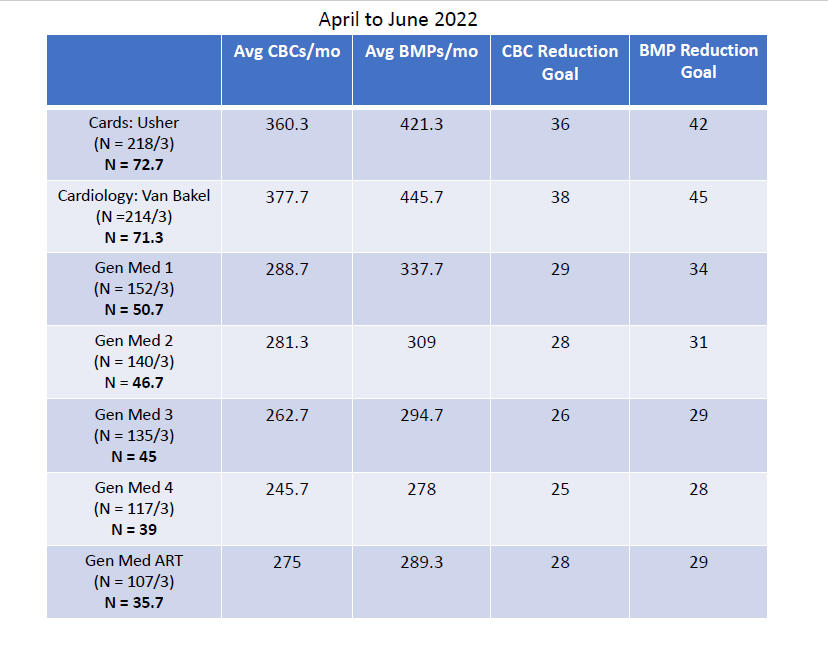
Description: EHR-generated reports are used to identify the number of laboratory tests ordered at the service team level. Service team is defined as the patients’ team at time of admission. Total lab tests ordered were calculated per service team over three month increments to allow for interventions to take effect. Baseline data was collected from April 2022 through June 2022 at the service team level. The interventions were developed by residents at monthly meetings in their academic time. The following interventions were developed and implemented from July 2022 through September 2022: (1) Presentation of the project at the attending hospitalist monthly meeting to raise awareness, (2) Reminder email to specialty physicians who work with residents on the wards, (3) Posted data sheets in resident work rooms, (4) Reminder cards on workstations, and (5) an organized competition amongst the teams to reduce the number of labs ordered monthly. We reviewed the data monthly and created a chart to track each service team, updating teams monthly.
Conclusions: This project is ongoing, with final results due in March 2023. Internal medicine residents are actively participating in quality improvement that affects the hospital as a whole. Residents design and implement various interventions and directly see the results of those interventions. Patients benefit from fewer lab draws based on the well-established side effects from frequent lab draws. Finally, the hospital benefits from reduced cost and personnel use to obtain daily labs.