Background: Mortality rates are a critical quality metric for hospitals, influencing both clinical outcomes and institutional reputation. The Centers for Medicare and Medicaid Services (CMS) incorporates 30-day mortality rates into its Value-Based Purchasing (VBP) program and Star Ratings, directly impacting hospital reimbursement and public perception. Similarly, U.S. News & World Report factors 30-day mortality into its rankings, and benchmarking organizations like Vizient use in-hospital mortality as a key component in assessing hospital performance. Improving mortality rates can therefore improve not only patient outcomes but also reimbursement and reputation.
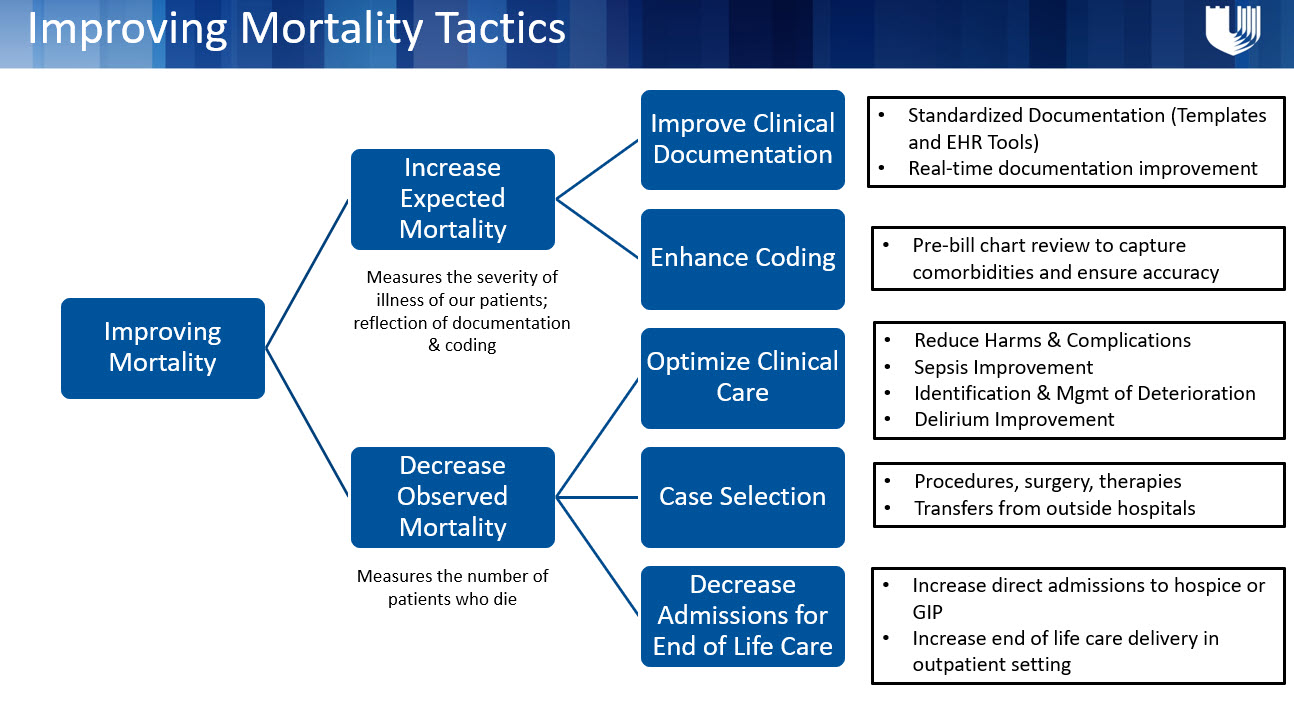
Purpose: Duke University Hospital had been absent from the U.S. News & World Report rankings since [insert year]. A key factor contributing to this decline was poor performance in the mortality domain. In response, our hospitalist- led Mortality Review Team initiated a focused effort to improve mortality outcomes within the general medicine service line. Given that the hospital medicine team manages a significant proportion of the patient population at Duke, we hypothesized that improving outcomes on our service line would lead to broader hospital-wide improvements in mortality. To address this, we developed targeted strategies to enhance both the observed and expected components of the mortality metric.
Description: To address observed mortality, we implemented several key interventions: the expansion of duties of a hospitalist-run Rapid Response Team, the establishment of an Opioid Use Disorder (OUD) Consult Team, and the development of a hospitalist-led Hospice and Comfort Care Team. These initiatives aimed to provide timely, targeted care to high-risk patients and improve overall patient outcomes. To enhance expected mortality, we focused on improving documentation processes. We introduced a standardized template for History and Physicals (H&Ps) and discharge summaries, which included automated prompts for commonly overlooked variables that affect patient complexity. Additionally, we integrated tools within the H&P and discharge summary to better capture less frequently documented factors that contribute to mortality risk such as coagulopathy and functional quadriplegia. Over the five-year period, more than 90% of admission encounters and discharge summaries utilized these enhanced documentation templates. The OUD consult team’s analysis showed a notable reduction in mortality among patients who received their intervention. Additionally, the rate of General Inpatient (GIP) conversions significantly increased. From fiscal year 2020 to fiscal year 2024, our hospital medicine mortality ratio decreased from 0.46 to 0.29, representing a 36% reduction in mortality over the five-year span.
Conclusions: The multi-faceted approach implemented by our Hospital Medicine Mortality Team resulted in significant improvements in mortality outcomes at Duke University Hospital. The combination of targeted clinical interventions, enhanced documentation practices, and improved care coordination led to a 36% reduction in our hospital medicine mortality ratio over five years. This culminated with a return to the rankings of Top Hospitals in US News and World Report in July 2024. These results underscore the importance of comprehensive, hospitalist-led strategies in improving patient outcomes and enhancing hospital performance in key quality metrics.