Background:
Nurse-Physician communication around discharge ensures that essential information is conveyed to patients when they leave the hospital. Yet nurses and physicians report poor communication during this critical time. The aim of this study was to standardize nurse-physician discharge communication through a resident-led intervention of a “Discharge Time-Out” (DTO).
Methods:
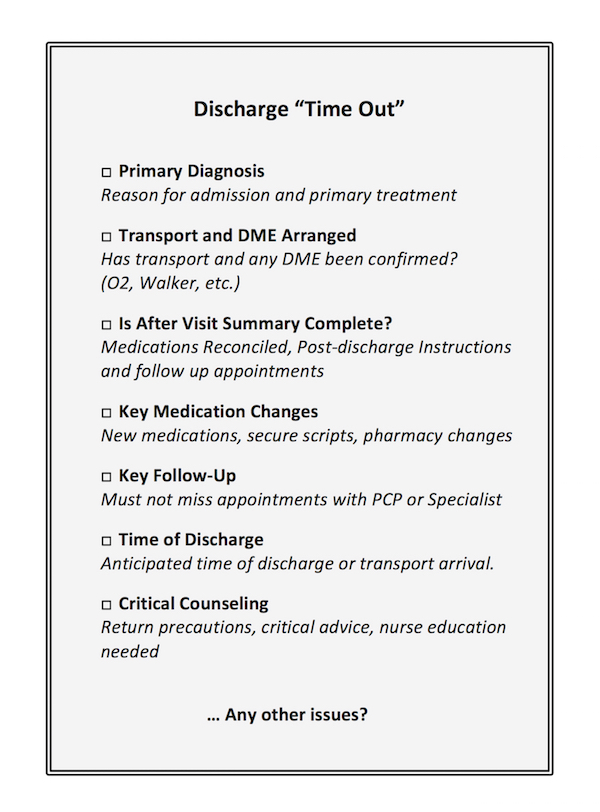
Previous surveys of nurses and physicians at our institution revealed poor communication around the elements of patient education at the time of discharge. A needs assessment of elements to include in the standardized communication was conducted using patient comments from an institution-wide post-discharge phone call. Analysis of the calls identified poor patient understanding of 1) new medications 2) discharge Instructions and 3) follow up appointments. Focus groups with nurses revealed lack of clarity around the discharge diagnosis and nursing education needs. Based on these results, a verbal communication checklist—the discharge timeout —was developed through nursing and resident collaboration. The final checklist was comprised of seven elements critical to safely discharging patients from the hospital (Figure 1). From February 2015 through June 2015 we surveyed nurses regarding their satisfaction with discharge communication on one medical unit involved in the DTO intervention. Nurses were asked if communication with the primary team occurred prior to discharge and if the DTO framework was used and were also asked to rate their satisfaction with the communication on a 0-10 scale.
Results:
Discharge communication and nursing satisfaction were assessed in 652 discharges. 567 (87%) discharges involved some type of physician-nursing communication. The average nursing satisfaction score was 8.15 when any reported physician-nursing communication occurred compared to 5.26 with no communication (P = <0.001). 271 (42%) discharges used the specific DTO framework. Use of the DTO framework was associated with a significant increase in nursing satisfaction compared to other verbal communication (8.91 vs 7.47, P<0.001).
Conclusions:
A standardized process promoting verbal communication between physicians and nurses at time of discharge improved nursing satisfaction with patient discharges. We are working to imbed the DTO into current discharge workflows and studying the impact on readmissions and patient satisfaction.