Background: Failures in communication among healthcare personnel are known threats to patient safety. Communication is particularly vulnerable to error when patient care responsibility is transferred from one provider to another (i.e., handoff). In this study we implemented a web-based handoff tool and provider training, and evaluated the impact on preventable adverse events (AEs).
Methods: We performed a prospective cohort analysis of patients on any of 3 general medicine or 2 general surgery teams before and after implementation of a web-based handoff tool and provider training. Patients were eligible for inclusion if they were cared for by any of the participating teams between November 1, 2012-February 1, 2013 (Time period 1, pre-implementation), April 1-June 18, 2013 (Time period 2, post-implementation), or November 1, 2013-February 1, 2014 (Time period 3, post-implementation). Between Time periods 2 and 3, Medicine services additionally underwent restructuring to regionalized care teams, daily admitting, and scheduled handoffs between day and evening teams. Surveys to screen for potential AEs were administered during the 3 time periods to nightfloat interns following their shift (to evaluate end-of-shift handoffs), and residents and attendings two days after starting on service (to evaluate end-of-service handoffs). Positive survey responses triggered chart review to determine presence and preventability of AE, harm level and attribution of AE to failure in communication, using previously validated scales. Ratings were adjudicated by trained physicians. We performed Poisson regression to obtain incident rate ratio (IRR) of preventable AEs per 100 patient-days in time periods 1 vs time periods 2+3, accounting for clustering by provider and controlling for service and patients’ demographics, length of stay, and comorbidities. Secondary outcomes included comparison of preventable AE rates in each time period, by service, and attributable to communication issues.
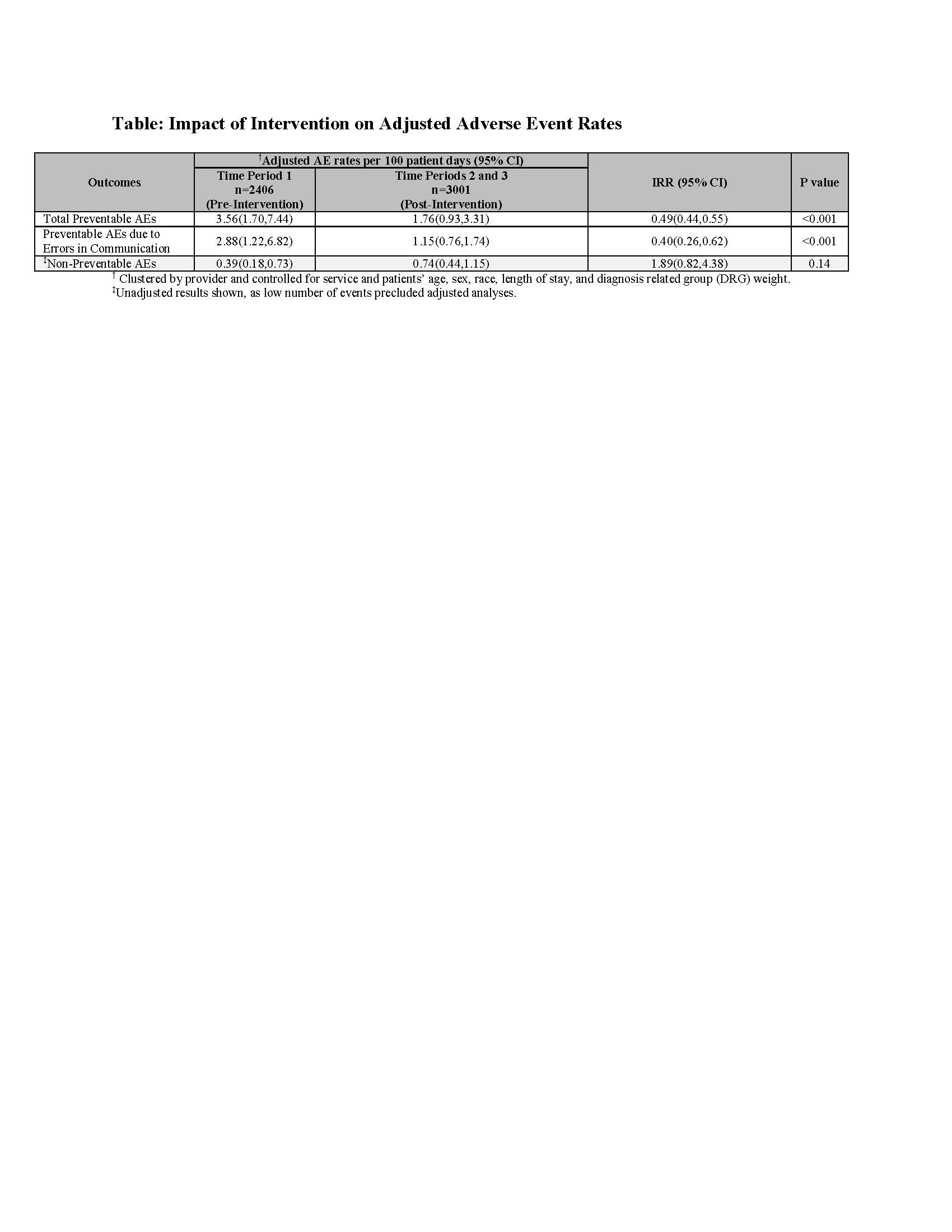
Results: Of the 5407 included patients, adjusted preventable AE rates per 100 patient-days significantly decreased from 3.56 in Time period 1 to 1.76 in Time periods 2 + 3 combined (IRR=0.49, 95% CI 0.44,0.55), and AEs due to communication failures decreased by 60%, while no difference was seen in non-preventable AEs (Table). Subgroup analysis showed additional reduction in AE rates on medical services between Time periods 2 and 3 from 1.84 to 0.74 (p=0.04).
Conclusions: We found that implementation of a web-based handoff tool and provider training significantly decreased preventable AE rates, including those due to communication failures. The additional benefit seen on medicine services between Time periods 2 and 3 may have been due to an additive or synergistic effect of restructuring of medical teams.