Background: : Low patient satisfaction can result in financial loss for hospitals, and potentially for individual physicians or groups and patient satisfaction is known to be lower on academic services.1 Increasingly, Medicare funds will be withheld from hospitals for underperformance in patient satisfaction due to Value Based Purchasing (VBP). We identified a low performing, academic unit at UMASS Memorial Medical Center in the realm of physician communication on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). As part of a quality improvement project we developed an intervention that addressed some of the identified root causes of this poor performance. These included poor multidisciplinary coordination of teams, teaching-centric morning rounds, poor patient engagement, and a lack of training in health care provider behaviors that affect patient satisfaction for clinicians.
Methods: Using LEAN-methodology, we devised and implemented a new bedside rounding structure on one of our academic units, run by Hospitalists, over a 9 month period which included the following changes:
- Full presentation and plan development at the patient’s bedside and with his or her involvement in this discussion
- Presence of a multidisciplinary team which included the patient’s nurse, a clinical pharmacist, medical students, residents and the attending physician during these bedside rounds
While the new rounding structure continued, several 4 week (PDSA) cycles were developed to address other root causes of poor patient satisfaction including:
- Public posting of patient experience scores
- Focused resident education about patient satisfaction and its association with healthcare outcomes
- Patient engagement through unit orientation and patient pamphlets
Data was collected through patient surveys (completed verbally, with the help of hospital interpreters when needed) of both the experimental group (patients who had experienced these interventions) and a control group (patients cared for on the same unit at the same time who did not experience the interventions). The following questionnaire, validated in a previous study, was used: 2
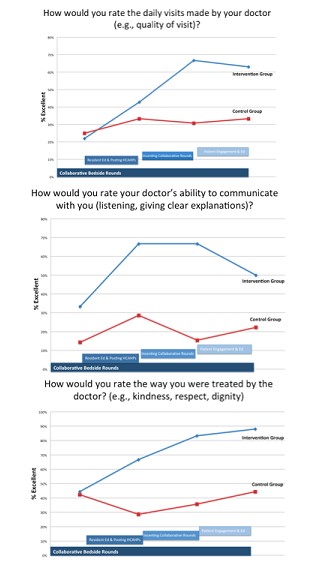
- How would you rate the daily visits made by your doctor (e.g. quality of the visit)?
- How would you rate your doctor’s ability to communicate with you (listening, giving clear explanations)?
- How would you rate the way you were treated by the doctor (e.g. kindness, respect, dignity)?
Results: We saw definitive improvement in physician communication metrics in the intervention patient groups when compared to the control groups at almost all of the assessment points and a trend toward improving scores over time. (See Figure 1.) Additionally, the unit-based, physician communication HCAHPS scores improved when compared to the prior year.
Conclusions: Adjustment in the work flow of an academic hospital unit and multidisciplinary interventions can positively affect patient satisfaction in the realm of physician communication.
1.) Shahian et al. Contemporary Performance of US Teaching and Nonteaching Hospitals. Academic Medicine Vol. 87 ; No 6, June 2012
2.) Dicther, J and Simone, K. Tools and Strategies for an Effective Hospitalist Program. Copyright 2006, HCPro, INC. ISBN 1-57839-766-9