Background: Nearly 6 million pediatric patients are discharged from the hospital yearly in the United States (AHRQ 2012), and social determinants of health (SDoH) impact discharge outcomes (Nacht 2022). Effective discharge planning prevents patient readmissions (Shapiro 2021), but the literature on how best to educate pediatric trainees is limited (Key-Solle 2010, Widmer 2015). We assessed the impact of a discharge planning workshop on pediatric residents’ reported self-efficacy in discharge planning and ability to generate an SDoH-informed discharge bundle.
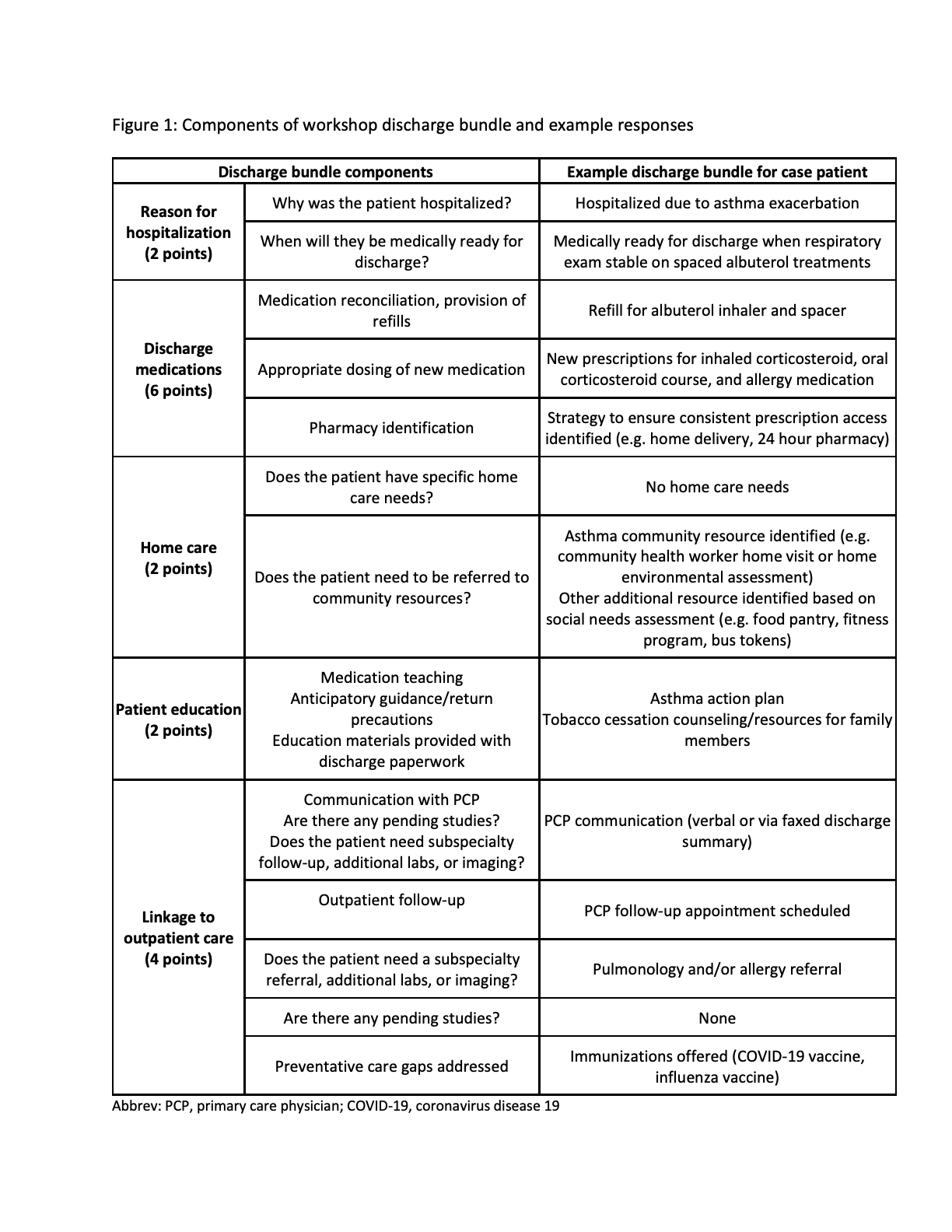
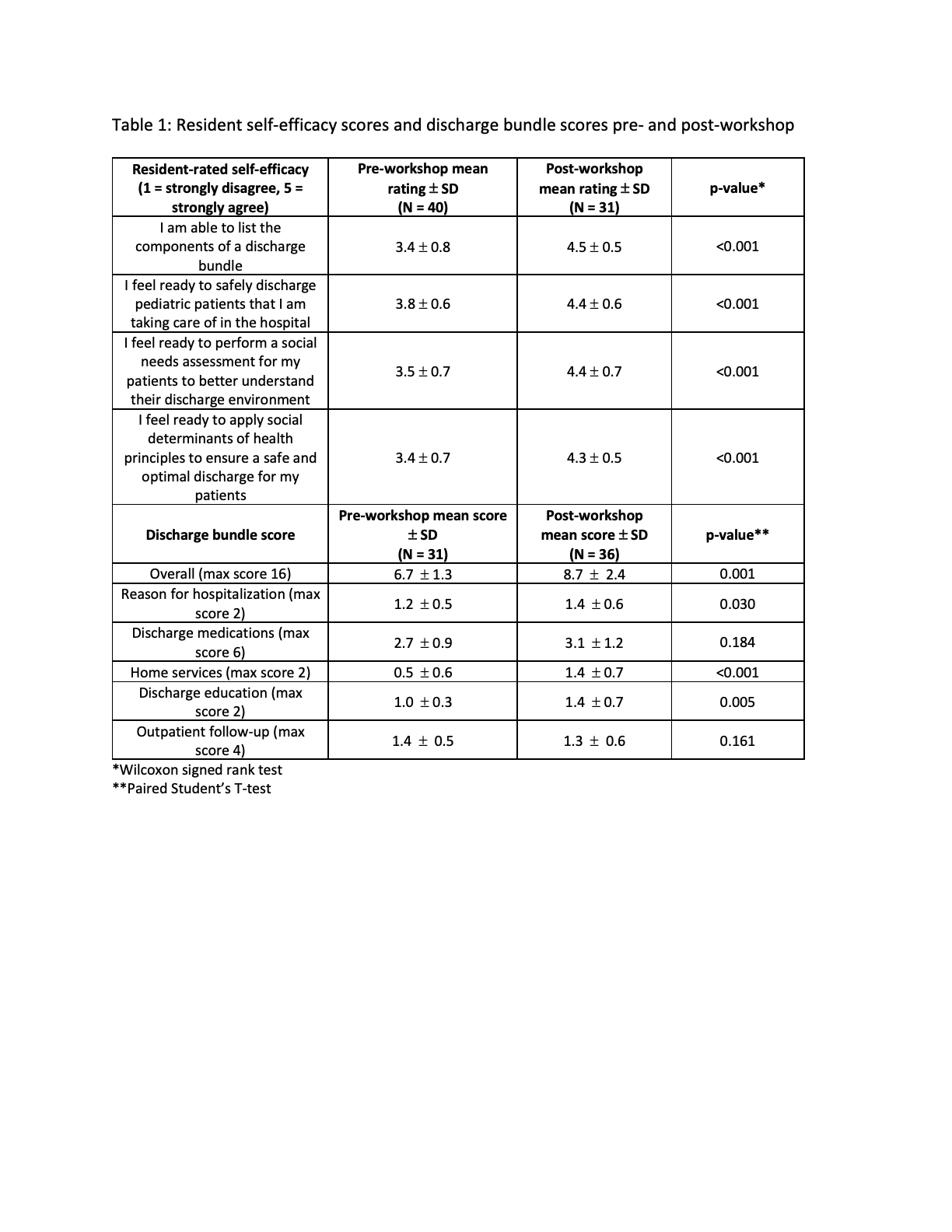
Methods: Pediatric residents (postgraduate years 1 & 2) participated in a one-hour discharge planning workshop during their 4-week inpatient community pediatrics and nursery rotations between January and November 2022. Immediately before the workshop, residents completed a pre-survey that included baseline resident characteristics, prior experience with discharge planning education, and reported self-efficacies with discharge planning (rated on a 5-point Likert scale: 1 = strongly disagree; 5 = strongly agree). During the workshop, residents first identified the components of a discharge bundle (modified from Soong 2013) and then developed an SDoH-informed discharge bundle for a case patient in which they 1) completed an initial discharge bundle, 2) completed a social needs assessment, and 3) incorporated the screen findings into a final discharge bundle for the case patient (Figure 1). Initial and final discharge bundles were submitted in real time during the workshop. Residents then completed a post-survey reporting self-efficacies and attitudes post-workshop. Resident discharge bundles were scored by an independent coder for completeness relative to a reference discharge bundle. Differences in pre- and post-workshop self-efficacy and discharge bundle scores were assessed with Wilcoxon signed rank test and paired Student’s T-test, respectively. Two-tailed P-value of < 0.05 was considered significant. The study was acknowledged as exempt by the Johns Hopkins Medicine Institutional Review Board (IRB00312106).
Results: Forty residents participated in the workshop and study. Self-efficacy improved across all measures, and discharge bundle scores were significantly higher post-workshop (mean score 6.7 +/- 1.3 vs. 8.7 +/- 2.4, p = 0.001; Table 1). 100% of participants agreed or strongly agreed that the workshop improved their understanding of discharge planning and that they will apply the framework from the workshop to future discharges.
Conclusions: Baseline self-efficacy for discharge planning activities, including incorporating SDoH, was low but improved with a brief workshop that taught residents to use a discharge bundle and SDoH screen. Discharge bundle completeness improved with use of the SDoH screen. Next steps include assessment of the replicability of our findings and impact on patient care.