Background: Academic medical centers (AMCs) have experienced significant clinical growth and have responded to the increase clinical demand by growing the number of hospital medicine services.[1,2] While this unprecedented growth has occurred, it has often outpaced the growth of housestaff training programs which has led to academic hospitalist teams evolving their clinical and educational models in a variety of ways.[2] We aimed to understand how hospitalist teams have evolved their clinical and educational models and the impact these strategies have had on their teams.
Methods: We conducted semi-structured interviews via virtual video with hospitalist leaders (including Division Head, Section Head, educational leaders) at different AMCs across the nation. Inclusion criteria included AMCs with 200 or greater beds hospital, AMCs with teaching as a central mission area and AMCs experiencing clinical growth. Clinical growth was broadly defined as an increase in total patients, an increase in hospitalist teams, or addition of hospitalist to the group in the last five years. Interviews focused on: (1) impact of clinical growth on educational growth; (2) strategies utilized to mitigate disproportionate clinical growth and increase educational growth; and (3) impact of these strategies. Interviews were audio-recorded, transcribed, and coded. A mixed inductive and deductive method at the semantic level was utilized to identify themes and subthemes.
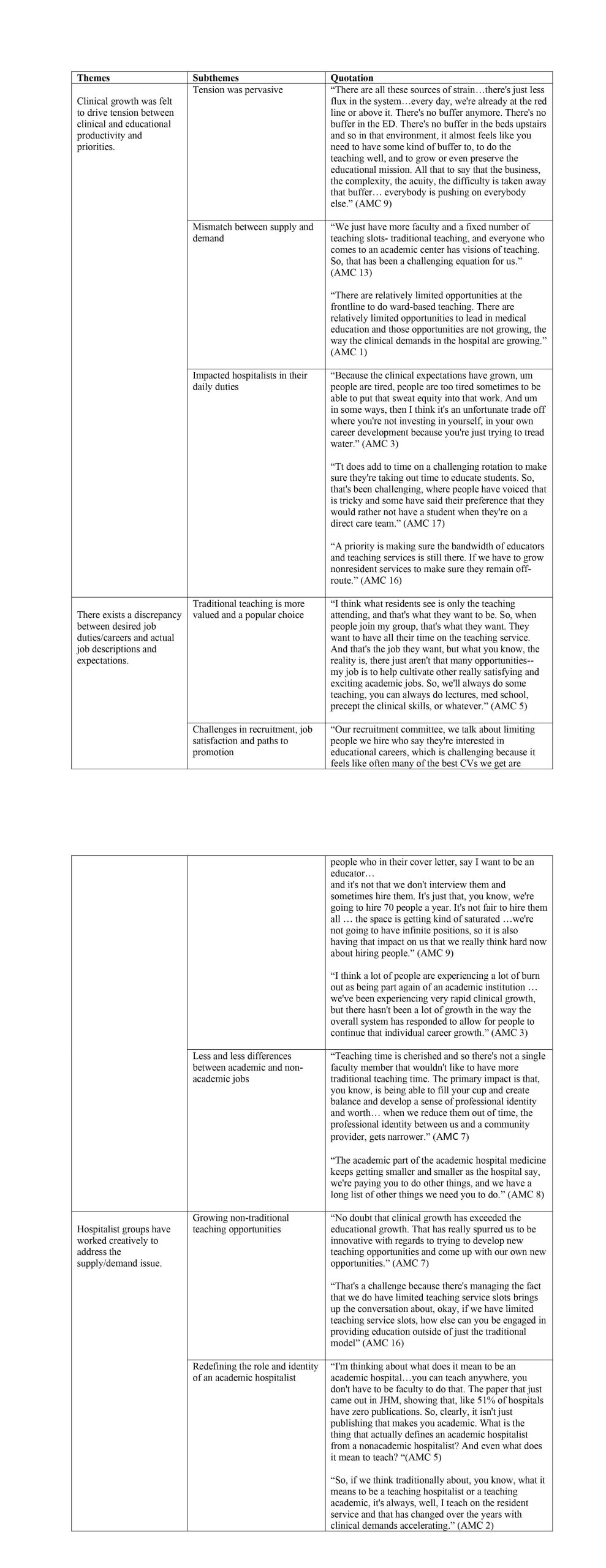
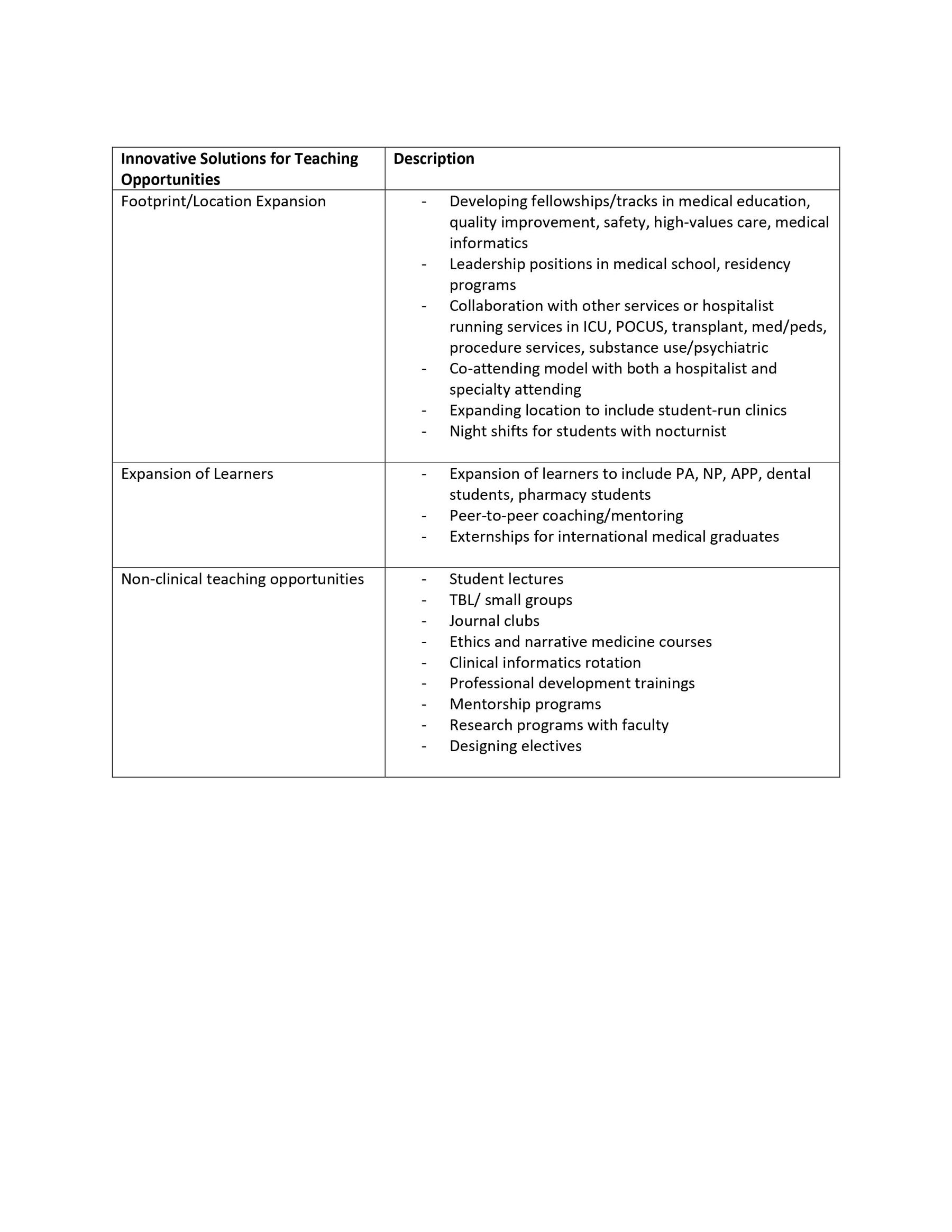
Results: From September 2021 to January 2022, 17 hospital medicine leaders representing 17 AMCs participated in the interviews. Three key themes were identified. (1) Clinical growth, both defined by volume and acuity, was felt to drive tension between clinical and educational productivity and priorities. This tension was pervasive at all sites, impacted hospitalists in their daily duties and created a mismatch between supply and demand for educational opportunities. (2) There exists a discrepancy between desired job duties/careers and actual job descriptions and expectations. Traditional teaching careers were noted to be popular and more valued choices among young as well as experienced hospitalists. Limited traditional teaching opportunities have created challenges in recruitment, sustaining job satisfaction, and paths to promotion. Academic hospitalists jobs have increased in their requirements for clinical duties leaving less differences between academic and non-academic jobs. (3) Hospitalist groups have worked creatively to address the supply/demand issue. Models utilized to distribute teaching roles included merit-based models (i.e., based on evaluations), equity models (i.e., teaching required and shared equally), and self-nominate models (i.e., self-elect into teaching). Each model had its pros and cons with none identified to solve the supply and demand problem. Hospitalist groups, however, found some success by focusing on growing non-traditional teaching opportunities and thinking about the role and identity of an academic hospitalist beyond the traditional teaching capacity, noting, some of these opportunities are threatened by the increasing drive for higher clinical productivity.
Conclusions: The hospitalist field faces supply and demand problems in both the clinical and educational settings driving a need to rethink educational opportunities. Solving the supply and demand problem presents a challenging problem to solve with no optimal solution.