Background: Physician handoffs between inpatient shifts influence safety and care quality. Handoffs are also at risk for communication failures. Poor care coordination and miscommunication cause 80% of sentinel events nationwide. The rise of the electronic medical record (EMR) presented an opportunity to standardize communication during handoffs. Unfortunately, this potential has thus far gone largely unrealized, due to the challenges of entering and retrieving summary patient information from the EMR in a way that aligns with clinical workflow. To address this shortcoming of the one-size-fits-all EMR, Trinity Health deployed an EMR-embedded rounding and handoff application (CORES, TransformativeMed Inc., Seattle WA) that organizes patient information in a specialty-specific way for handoffs, as well as rounding and pre-rounding workflows.
Purpose: The purpose of this study was to investigate physician’s perceptions of clinical workflow efficiency with traditional methods for communicating during rounds and handoffs, and how CORES impacts this process, and ultimately impacts patient safety and physician satisfaction.
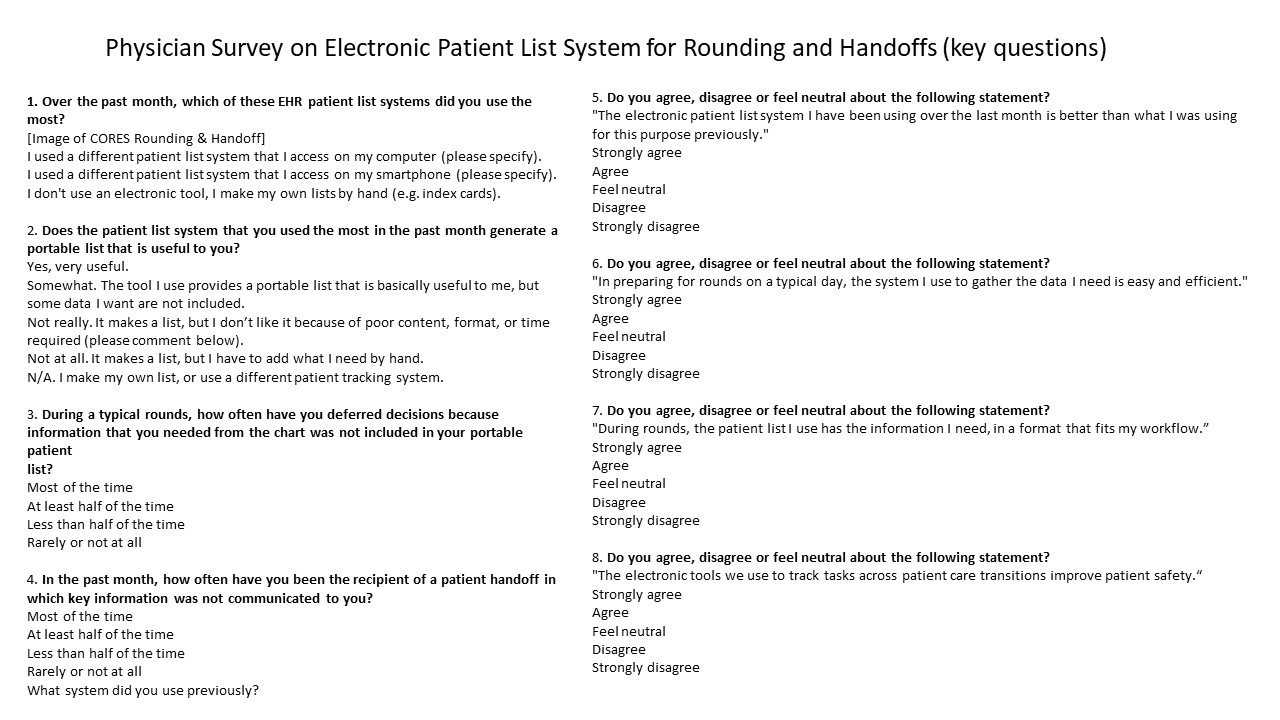
Description: An anonymous email survey was sent to inpatient physicians between January 30th and March 19th, 2018. Recipients included attending physicians, residents, and advanced practice providers in multiple specialties. Responses were obtained from two groups: CORES users and non-CORES users. CORES users were defined as using CORES for greater than 1 week, including using patient lists generated by CORES for rounds. Non-CORES users had used CORES for less than 1 week, or not at all. Questions were focused on views of EMR patient list usefulness, patient safety, pre-rounds preparation, rounding efficacy, and handoffs. Because of the stage of CORES implementation and dissemination at the time of the survey, CORES users were more common than non-CORES users. 161 survey responses were collected from CORES users (n=127) and non-CORES users (n=16). Patient safety was perceived to be improved, with 62.2% of CORES users indicating that they agree, or strongly agree, that the electronic tools used to track tasks across patient care transitions improve safety. Information needs during pre-rounds preparation, rounding and handoffs were reported to be better with CORES (by 68.2%, 68% and 87.5%, respectively). Physicians’ satisfaction with EMR-generated lists was also found to be improved.
Conclusions: Implementation of an EMR-embedded application to better serve physicians’ information needs during handoffs and rounding was viewed to be an improvement by providers. More specifically, this data suggests the tool was perceived by the majority of providers using it to have made a positive impact on patient safety, pre-rounds preparation, rounding, and handoffs.