Background: Implantable cardioverter defibrillator (ICD) shocks can be traumatic for patients and families, particularly at the end of life. Studies estimate between 51-65% of ICDs remain active at time of death, with 24-31% of patients receiving shocks within the last day of life, and 8% in the last minute of life. The Heart Rhythm Society (HRS) states that physicians are obligated to discuss whether a patient’s device therapy is in line with goals of care, particularly when there is a change in code status. While physicians believe they should engage in these conversations with patients, they rarely do.
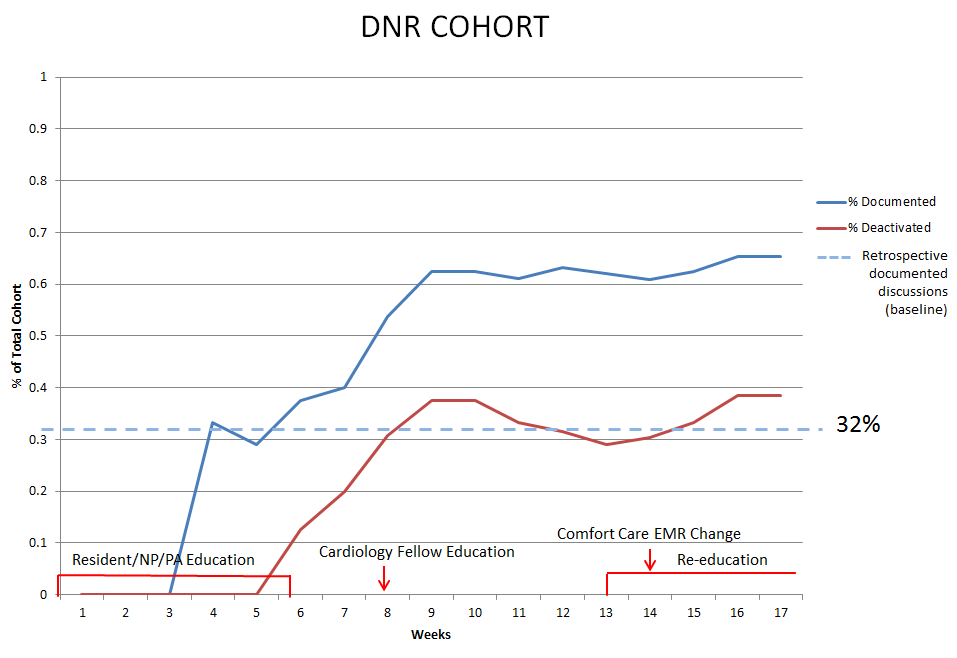
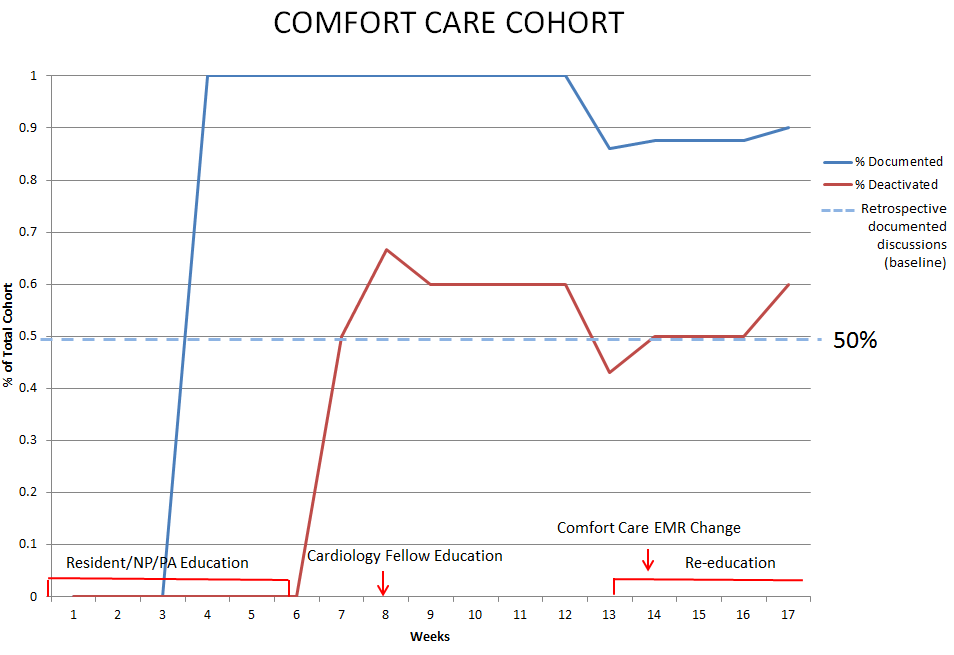
We retrospectively examined patients made DNR and/or comfort care while admitted to medicine services at New York Presbyterian Hospital Weill Cornell Medical Center (NYPH-WCMC) from Dec 1, 2017 to May 30, 2018. Amongst comfort care, only 10 of 20 patients (50%) and within DNR only 14 of 41 patients (32%) had documented discussions and/or deactivated ICDs at the time of death or discharge.
In line with published guidelines, we designed a project to increase the frequency of documented discussions regarding ICD therapy at the time of DNR or comfort care decisions through education and EMR changes.
Methods: The study executes weekly Plan-Do-Study-Act (PDSA) cycles with data collection every Friday. There will be 28 total PDSA cycles (six months). Only patients admitted to medical services at NYPH-WCMC are included, as our interventions mostly target providers within medicine departments. Patients admitted with already deactivated ICDs are excluded.
To date, we have performed 17 of 28 PDSA cycles. Education sessions and pre- and post-knowledge surveys were given to medicine residents and physician assistants (weeks 1-6), and cardiology fellows and nurse practitioners (week 8). The decision support tool was embedded within the comfort care order (week 14). A reminder alert for DNR documentation will be implemented (week 18). We also plan on educating hospitalists (week 19), distributing a hospital-wide email, creating posters and patient pamphlets, and speaking at RN work rounds.
Our primary outcome measures are percent of ICD recipients made comfort care with documented ICD discussions and percent of ICD recipients made DNR with documented ICD discussions. Our secondary outcomes are percent of ICD deactivation in each group and pre-, post-, and midpoint knowledge surveys.
Results: Since implementation, in the comfort care cohort, the rate of documented discussions and/or deactivated ICDs improved from 50% to 90% of patients (n=10). In the DNR cohort, this rate improved from 32% to 65% of patients (n=26). Accordingly, the rates of ICD deactivation increased from 45% to 60% in the comfort care cohort and from 29% to 39% in the DNR cohort. Zero patients have received undesired shocks from their ICDs during our study.
Conclusions: Standardized education of healthcare providers and incorporating decision support tools in the EMR are effective ways to increase awareness, discussion, and deactivation of ICDs in DNR or comfort care patients.