Background: Proton pump inhibitors (PPIs) have been associated with adverse events and increased mortality in patients diagnosed with cirrhosis (1). PPIs are commonly prescribed to patients with cirrhosis who present to the hospital with gastrointestinal bleeds (2). However, guidelines do not suggest routine usage of PPI in patients with cirrhosis without gastroesophageal reflux disease (GERD) or peptic ulcer disease. In this analysis, we evaluated the association between variceal bleeds and use of PPI in patients with end stage liver disease (ESLD) at the time of liver transplant evaluation (LTE).
Methods: We retrospectively analyzed 458 patients with ESLD undergoing non-urgent LTE. Subjects were categorized by 1) history of GERD (yes/no) and 2) PPI usage (yes/no). Ultimately 4 cohorts were defined: GERDPPI (n=119), GERDno-PPI (n=35), No-GERDPPI (n=145), No-GERDno-PPI. (n=159). Appropriate treatment included: 1) patients with GERD on a PPI (GERDPPI ) and 2) patients without GERD and not on a PPI (No-GERDno-PPI). We identified rates of liver related complications in each group and evaluated for an association between variceal bleed history and subject cohort using Chi Squared tests and logistic regression modeling. Analysis was completed in SPSS 29 and statistical significance was evaluated at p=0.05.
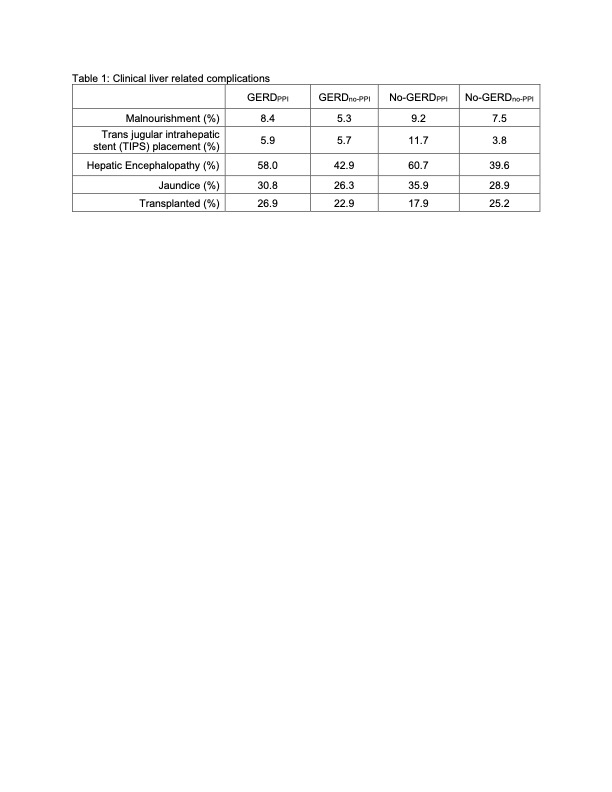
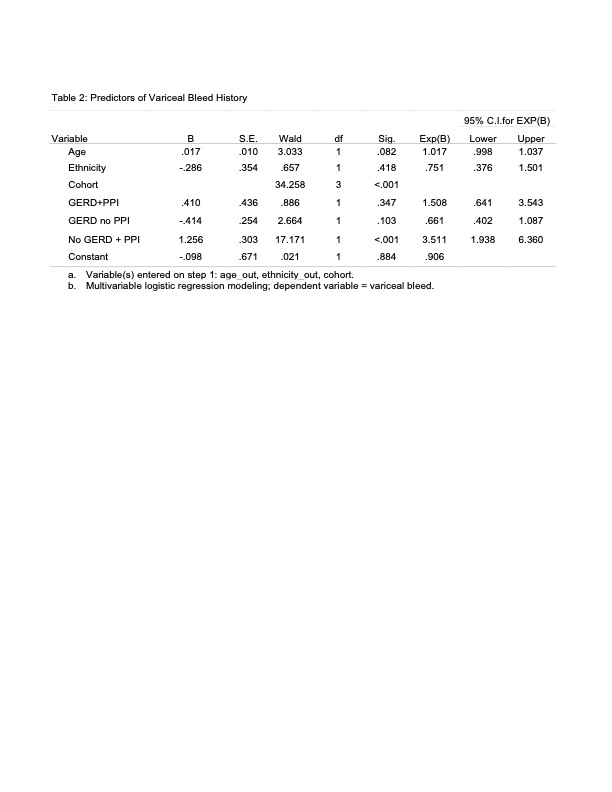
Results: One in three subjects (33.6%) had a documented diagnosis of GERD, but over half (57.6%) were on a PPI at the time of LTE. Over 75% of subjects GERD diagnosis were appropriately on a PPI, but ~ 50% of subjects without a GERD diagnosis were inappropriately on a PPI (n=145). Overall, PPI use was associated with a history of variceal bleed compared to no PPI use (40.2% vs. 15.9%, p< 0.001). Rates of common complications of liver disease including hepatic encephalopathy, jaundice, TIPS placement, and malnourishment were highest and transplant rate was lowest in No-GERDno-PPI subjects (Table 1). When controlling for age and ethnicity, subjects without a diagnosis of GERD on a PPI were 3.5 times as likely to have had a variceal bleed (Table 2).
Conclusions: Our analysis demonstrated patients with cirrhosis and variceal bleeds often end up on long-term PPI. Further, we observed increased liver related complications and decreased transplantation in patients on PPI without indication (No-GERDPPI). While our study was unable to assess a temporal association, this data could indicate that 1) PPIs may worsen outcomes in patients with chronic liver disease, especially when used without indication and 2) failing to discontinue PPIs when appropriate could drive worse patient outcomes. Ultimately, providers should carefully consider use of PPI when caring for patients with end stage liver disease awaiting liver transplantation.