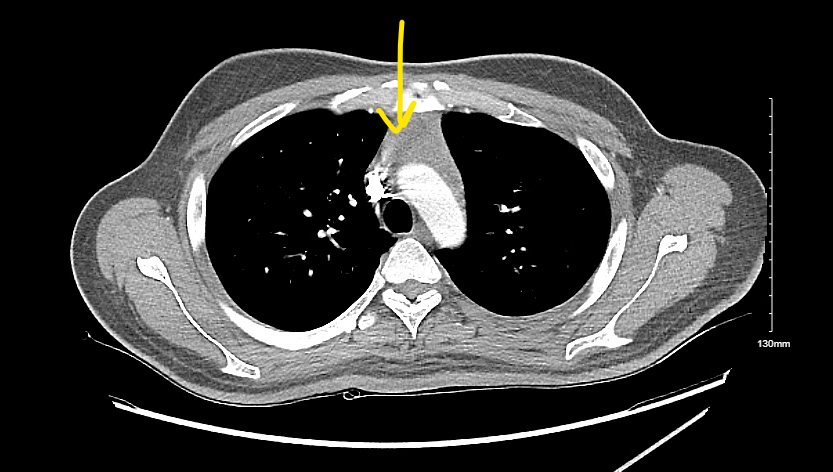
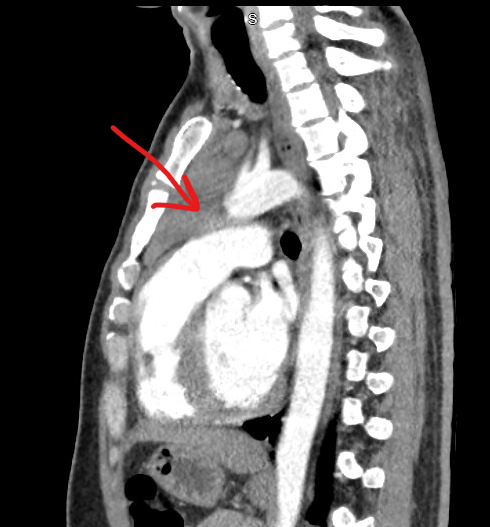
Case Presentation: A 30 year old male presented with symptoms of intermittent episodes of chest pain with palpitations, tremors associated with night sweats, heat intolerance, and unintentional weight loss for the last 6 months. He had no significant past medical history, did not take any medications at home, and had no prior surgeries. He denies a history of excessive alcohol use, smoking, or any recreational drugs. His exam revealed a borderline tachycardia rate of 90 with a small diffuse goiter. He had no cervical or axillary lymphadenopathy and he had tremors on outstretched hands. Initial investigations revealed unremarkable complete blood count and comprehensive metabolic panel. His thyroid panel revealed undetectable TSH (< 0.01), free T4 was 7.30, and TSI of 12. His imaging revealed a large lobulated mass in the anterior mediastinum measuring 6.1x6.2x2.4 cm. The patient was started on propranolol and methimazole for Graves disease. IR-guided biopsy of the mediastinal mass revealed a small fragment of normal thymic tissue and was negative for any tumor markers.
Discussion: Anterior mediastinal mass includes a broad differential ranging from benign pathologies to malignant germ cell tumors. Due to this broad differential, correlation with the epidemiology of these lesions and the patient’s age, gender, clinical symptoms, radiologic features, and comorbidities can aid in the diagnosis. A needle or excisional biopsy is not always required for diagnosis. Thymic hyperplasia (TH) refers to gross symmetric enlargement of the thymus. TH is associated with multiple autoimmune diseases, most commonly reported with Graves disease, systemic lupus erythematosus, myasthenia gravis, and progressive systemic sclerosis (1,2,3). Association of Graves with thymic hyperplasia was described back in 1912 (4,5) with numerous case reports thereafter as an incidental mediastinal mass on chest imaging. Graves disease is an autoimmune disease characterized by autoantibodies that activate thyrotropin receptors (TSHR) and stimulate thyroid hormone production and growth of the thyroid gland resulting in goiter. The exact pathogenesis of TH is still ill-defined but proposed mechanisms include an absolute increase in the number of epithelial cells in the thymus in response to excess thyroid hormone resulting in thymic hyperplasia (6) with additional immunologic mechanisms due to the presence of Thyrotropin receptors in the thymus (7). Data from case series and systematic reviews of literature support the benign nature of TH associated with Graves with regression of thymic tissue in most cases with anti-thyroid medication, by up to 85% in 6 months. Factors associated with a benign nature are homogenous mass, no invasion of surrounding tissue, or calcification. In patients with favorable imaging findings, experts recommend a conservative approach with the treatment of hyperthyroidism and repeat imaging in 6 months, and further surgical intervention if the mass persists (8).
Conclusions: Although well-known to Endocrinologists, this association is under-recognized by general physicians. Lack of familiarity with this association and its benign course may result in invasive management including excisional biopsy and thymectomy along with its associated costs and harms.