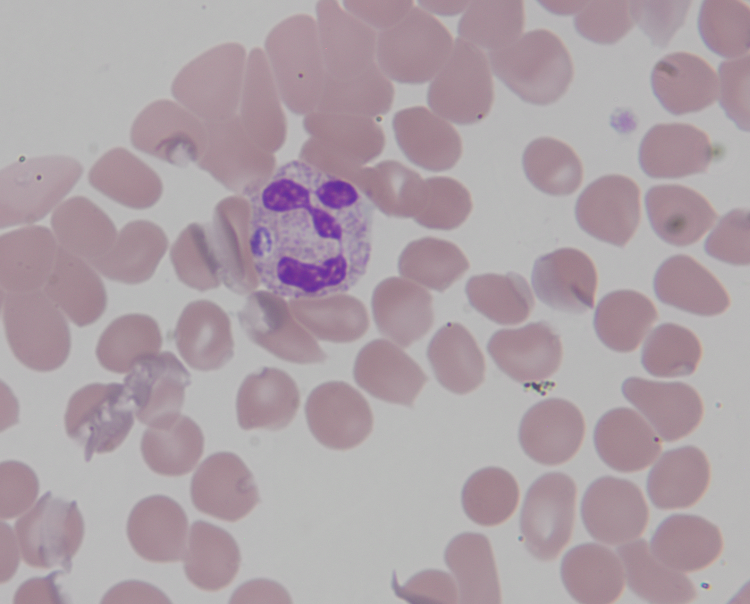
Case Presentation: An 81-year-old male presented in July with two months of recurrent fevers. He was initially hospitalized in early May for LLQ pain, diarrhea, and imaging findings consistent with diverticulitis and a small pericolonic abscess. He was discharged on ciprofloxacin and metronidazole with outpatient colorectal surgery follow-up. He required subsequent admissions in late May and again in late June for treatment of what was thought to be un-resolving diverticulitis. He was treated with IV piperacillin-tazobactam and discharged with oral amoxicillin-clavulanic acid. Despite broad coverage treatment for diverticulitis, he continued to have high fevers up to 39.4°C, a 7.9 kg weight loss, fatigue, sweats, chills, and mental status changes prompting a fourth admission in early July. Notably, his abdominal pain had resolved. Repeat CT abdomen showed stable sigmoid diverticulitis. He denied known tick bites but lives near the woods in a tick-endemic region of Pennsylvania. Laboratory analysis revealed thrombocytopenia (108), and acute kidney injury (Cr 1.7). Platelets had been progressively down trending from 429 in May to 89 in July on admission. CRP (9.91) and ESR (44) were both elevated. Imaging ruled out pneumonia and showed improved sigmoid diverticulosis. Given the treatment-resistant fevers and new thrombocytopenia, doxycycline was initiated to cover for any tickborne illness and broad-spectrum antibiotics for diverticulitis were continued. Peripheral blood smear revealed very rare neutrophils with inclusion bodies suggestive of anaplasmosis. Anaplasma antibody IgG levels were elevated at 1:320. No significant antibodies against B. microti, E. chaffeensis, or Lyme were detected. Anaplasma phagocytophilum was detected by PCR, whereas Babesia and Ehrlichia species were not. His fevers resolved 48 hours after initiating doxycycline and thrombocytopenia improved by day 3 of admission. He was discharged on a 14-day course of doxycycline.
Discussion: The Ixodes scapularis tick, endemic to northeastern regions of the United States, is the predominant vector for Anaplasma phagocytophilum. The incidence of Anaplasma peaks between May and July, corresponding to the nymphal stage of blacklegged ticks (Ixodes scapularis). Survival of Ixodes hinges on environmental conditions within a range of 10°C to 35°C and humidity exceeding 80%. Nationally, the CDC reported an escalation in Anaplasma cases from 3659 (2015) to 5655 (2019). Remarkable increases were observed at the local level, particularly in Pennsylvania, where the incidence surged from 1.64 cases per million (2015) to 16.72 cases per million (2019).
Conclusions: Anaplasmosis, a tick-borne Rickettsial disease, typically presents with nonspecific symptoms of fever, myalgia, malaise, and headaches. Given the rising incidence of Anaplasmosis in the Pennsylvania region, especially during the summer months, the diagnosis should be on the differential when presented with patients with high, recurrent fevers and thrombocytopenia.