Background: Academic medical centers and other quaternary hospitals struggle with capacity challenges that manifest in longer ED wait times, delayed or cancelled elective surgical procedures, and delayed transfers from community hospitals[1]. The Hospital at Home model is an obvious and elegant solution to increase capacity[2], but its nationwide implementation has been limited due to lack of payor participation and uncertain future funding [3]. To address these limitations, in 2020 the University of Utah Hospital partnered with Community Nursing Services (CNS), a Utah-based home-health agency, to create University of Utah “Heal at Home.” Heal at Home moves post-operative and medical care for appropriate patients from the hospital to the patient’s home. Unlike hospital-at-home models, the Heal at Home model uses the home-health benefit already present in most health insurance plans and thus is not dependent on a novel payment mechanism for sustainability. To our knowledge, the vertical integration of a home health company within an academic medical center across multiple medical and surgical specialties as a targeted intervention to address inpatient capacity challenges in a fiscally sustainable manner has not been previously described.
Purpose: Heal at Home focuses on transitions of care to improve hospital capacity. Heal at Home uses pre-defined care pathways to facilitate abbreviated post-surgical and hospital stays and transition care delivery safely to the home. This program currently serves patients from Hospital Medicine, Emergency Medicine, Physical Medicine & Rehabilitation, and nine surgical specialties. Three other specialty specific programs are in development.
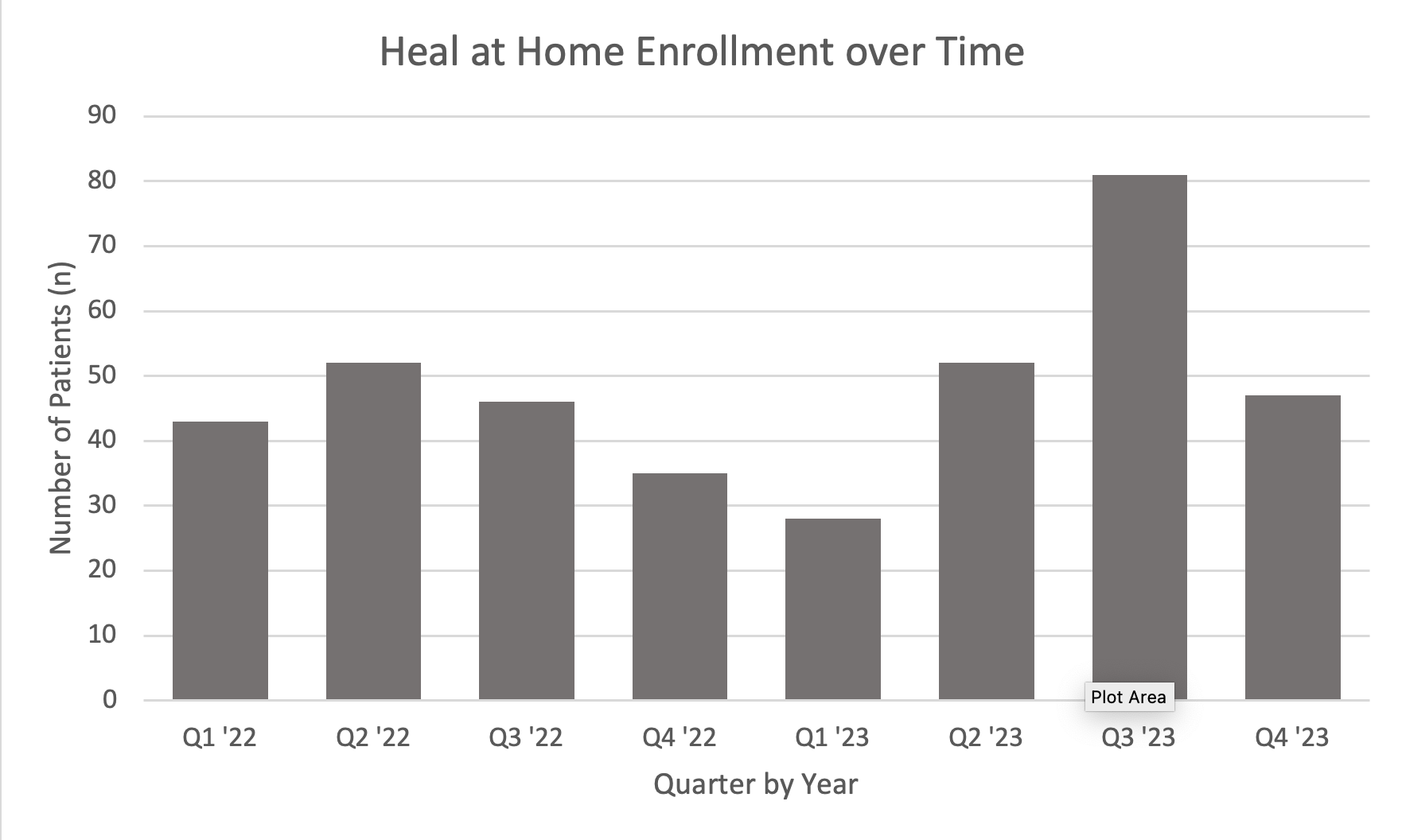
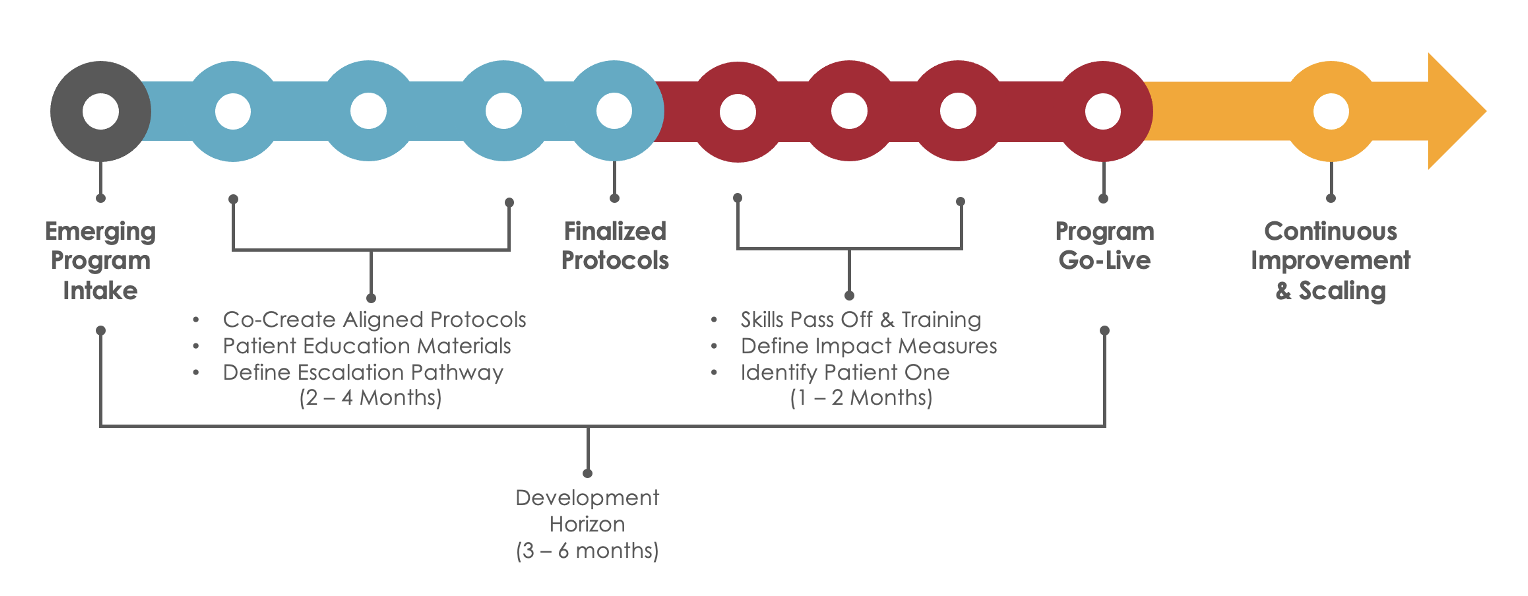
Description: The Heal at Home Core Team has representatives from physicians, case management, nursing leadership, CNS, data analytics, and population health. Early on, program participation was voluntary as individual providers approached the Core Team to help with departmental capacity constraints. Now that the program is mature, the Core Team prospectively identifies populations where hospital care could be safely transitioned to the home. Program development occurs during a 2-6 month period in which a provider-champion meets at regular intervals (2-4 weeks) with the Core Team to develop care protocols that address needs unique to their patients or procedure. The team establishes escalation pathways to allow for bidirectional communication between inpatient providers and home health personnel if needs arise after patients return home. Home health nurses receive in-person specialty specific training from providers and nurses in the specific needs for new patient groups. After program go-live, processes are regularly re-visited and adjusted to ensure a safe, sustainable, and patient-centered experience. Between January 2022 – November 2023 (23 months), 384 patients were enrolled saving an estimated 292 bed days. No patients have died while enrolled in Heal at Home. Patients experienced a 30-day ED visit rate of 10.4% (n=40) and an unplanned readmission rate of 6.8% (n = 26) compared to 30 day ED visit rate of 8.8% and unplanned readmission rate of 16.1% for all University discharges to Home Health agencies.
Conclusions: Heal at Home is a multi-disciplinary, multi-specialty program that allows patients to safely transition from the hospital to home. This model addresses health system capacity challenges by reducing length of stay while ensuring sustainability by using existing reimbursement mechanisms.