Case Presentation:
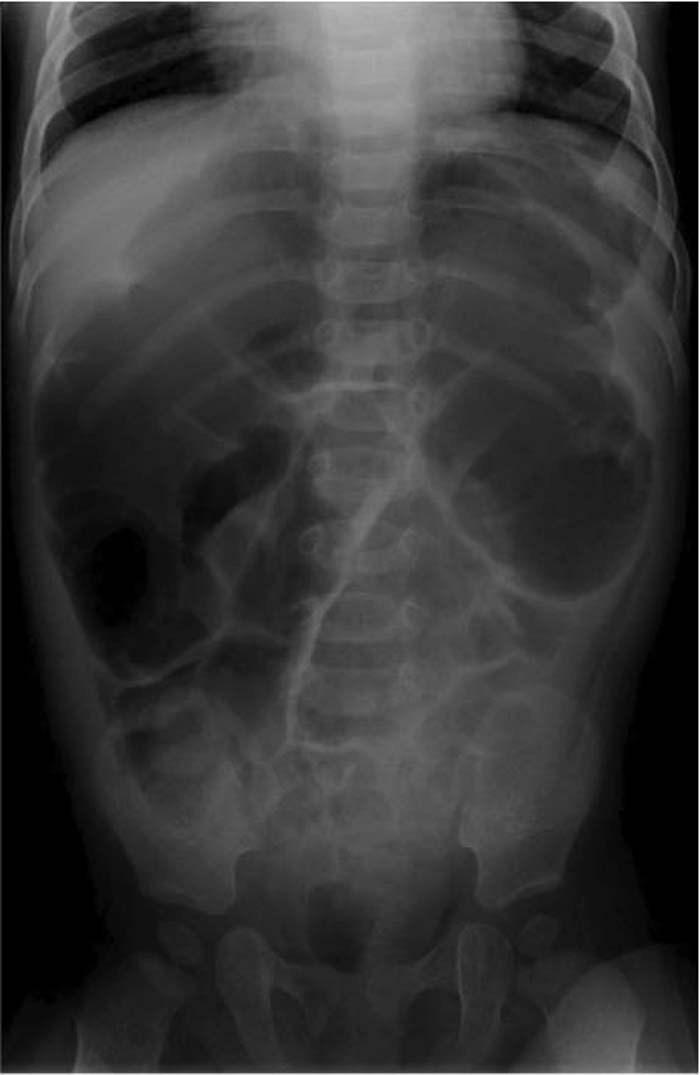
A 7‐month‐old healthy female infant presented to the emergency room with a 10‐day history of no stools. Her mother noted that she had a decreased activity level, decreased appetite, and abdominal distention and at times appeared to have abdominal pain. She did not have fever vomiting, or weight loss. Her diet strictly consisted of breast milk. There was no history of honey or corn syrup ingestion. Her previous stooling pattern had been within normal limits. The infant was afebrile, and her vital signs were stable. On physical examination, she was alert appearing and in no apparent distress, but her overall activity level was decreased. Her anterior fontanelle was flat. Her cardiac and pulmonary exam was normal. Her abdominal exam was notable for hypoactive bowel sounds but was otherwise normal. She had a patent anus with no stool palpable in the rectal vault. Neurologic exam was normal. At the time of presentation, her abdominal X‐ray was significant for distension of the large and small intestines. Over the duration of her 2‐week hospital course, she developed ptosis, sluggish pupillary response, increasing weakness, hypotonia, loss of DTRs, difficulty feeding, and lethargy. A workup, including blood, urine, and CSF cultures, thyroid studies, head CT, MRI, EEG, and rectal biopsy, was normal. EMG performed on hospital day 7 was abnormal but not considered significant enough to represent botulism toxicity. When a suitable stool sample was obtained on hospital day 9, it was positive for Clostridium botulinum toxin type B, although the previous stool and serum samples had both been negative. At the time of discharge she was clinically improving. Parents declined Baby Botulism Immune Globulin (BIG). The source of the toxin was thought to come from soil on a farm near the family home.
Discussion:
Infantile botulism is caused by a toxin produced by Clostridium botulinum. According to the CDC, there are an average of 110 cases of botulism reported in the United States each year. Infant botulism occurs when ingested C. botulinum spores colonize the digestive tract and produce botulism toxin. Most infants present with lack of defecation for more than 3 days, lethargy, weakness, hypotonia, poor feeding, or weak cry. Examination may reveal sluggish pupillary response, ptosis, flaccidity, lack of head control, weak gag reflex, or poor anal sphincter tone. Diagnosis may be made by nerve conduction studies or by detection in stool samples. The treatment is usually supportive, but human‐derived antitoxin, Baby Botulism Immune Globulin (BIG) Intravenous, has also been available since 2003.
Conclusions:
Infant botulism should be considered in all infants who present with several days of constipation, hypotonia, or poor feeding. All forms of botulism have the potential to be fatal and are considered medical emergencies. However, early diagnosis and supportive management are usually associated with decreased mortality and complete recovery.
Author Disclosure:
P. Newton, none; R. Kamat, none.