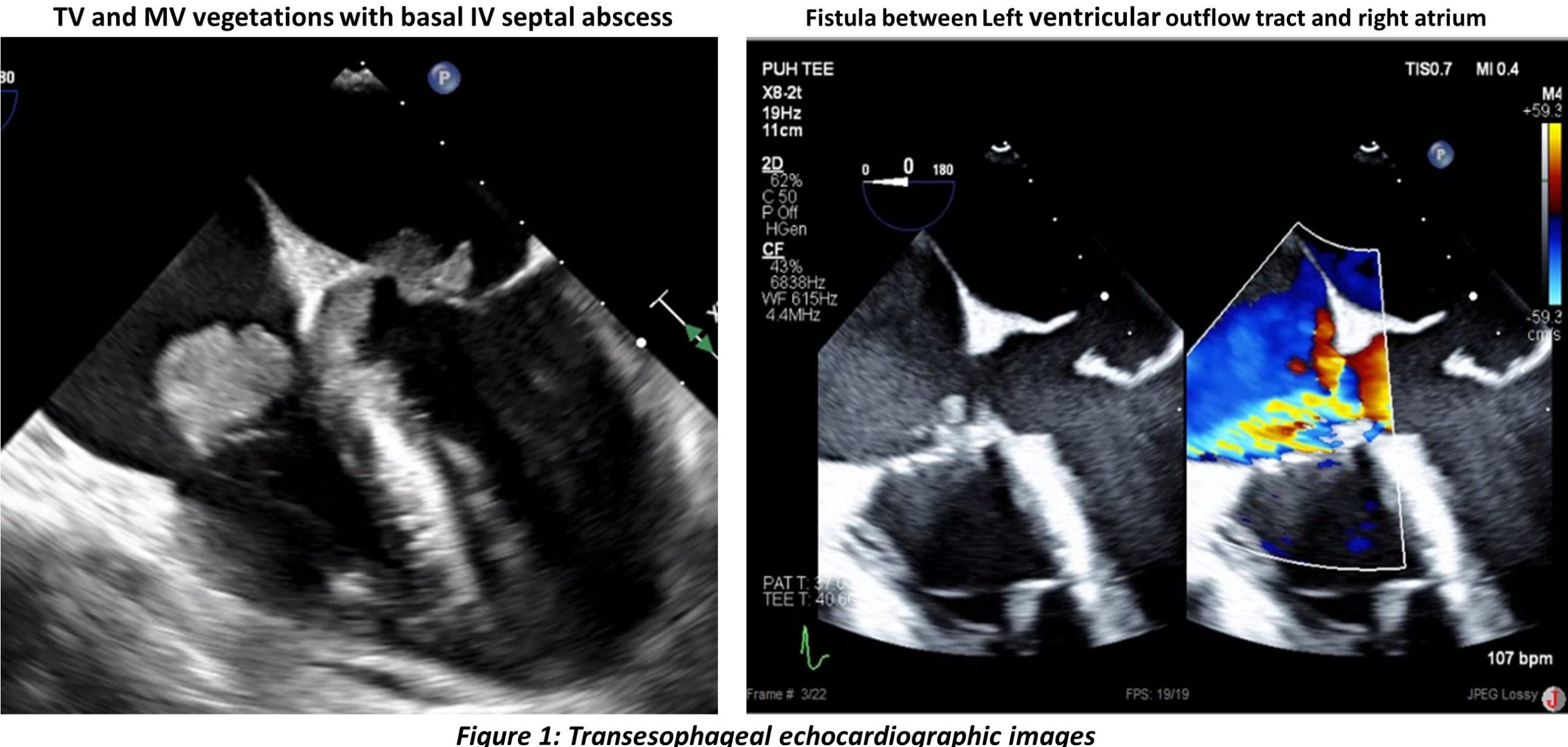
Case Presentation: A 29-year-old man with medical history of type 1 diabetes mellites complicated by chronic nonhealing diabetic foot wound presented with one week history of shortness of breath and malaise. On physical exam he was hemodynamically stable and had a new grade II/VI holosystolic murmur at lower sternal border. Initial laboratory workup revealed elevated leukocytosis, hyperglycemia and ketonemia. An EKG on presentation revealed a new complete heart block (CHB) with junctional escape rhythm and a heart rate (HR) of 50 beats per minute (bpm). History was unrevealing for nodal blocking agents, a TSH and lyme panel was unremarkable. Blood and right foot wound cultures grew methicillin sensitive staph aureus. Patient was started on treatment with intravenous oxacillin. Further workup with a transthoracic echo (TTE) revealed vegetations on the anterior leaflet of mitral valve (MV) and septal leaflet of the tricuspid valve (TV) in continuity with the basal ventricular septum representing an abscess. Subsequent transesophageal echocardiogram showed extension of vegetation to basal interventricular septum with abscess formation extending into the aortic annulus without fistula formation. His hospital course was complicated by development of confusion with right sided weakness. A computed tomographic (CT) angiographic scan of head and neck revealed multifocal ischemic infarcts. CT chest revealed bilateral pulmonary septic emboli and a CT abdomen and pelvis revealed splenic and bilateral renal cortical infarcts. Within few days he developed worsening symptomatic bradycardia with HR of 30 bpm. A follow-up TTE showed progression to perforation of anterior mitral annulus, with formation of left to right shunt between left ventricular outflow tract and right atrium. Immediate cardiothoracic surgical evaluation was obtained and patient underwent bioprosthetic MV replacement and TV repair along with fistula patch repair and placement of permanent dual chamber pacemaker. He had an uncomplicated post-operative course and was treated with six weeks of intravenous antibiotics.
Discussion: Infective endocarditis (IE) is rarely complicated by formation of an intracardiac fistula.(2) However when present, aorto-cavitary fistula is associated with higher incidence of conduction system disorders (1), and systemic embolization.(3) Perivalvular abscesses may complicate into intracardiac and pericardial shunts that are difficult to manage with medical management alone.(3) Some of the indications for surgery in endocarditis include peri-annular extension, systemic embolization and cerebrovascular events(4), which were present in our patient. AHA/ACC guidelines recommend early surgical intervention for patients with recurrent emboli and persistent vegetations.(5)
Conclusions: Presence of valvular complications in IE patients such as periannular extension warrants urgent surgical referral and repair, and should not be delayed due to risk of increased mortality in such patients.