Background: Hospital-Associated Disability (HAD) is a life-altering condition that can lead to readmissions and is associated with increased risk for death. Physical therapy (PT) is an invaluable tool to help prevent HAD but, studies have shown that even under normal circumstances, there are a multitude of barriers to adequate PT in hospitalized patients. The COVID-19 pandemic has the potential to significantly worsen these barriers. In this study, we aimed to assess physical and occupational therapists’ perceptions of working with inpatients during the COVID-19 pandemic.
Methods: We conducted a qualitative phenomenological study using semi-structured interviews. Email was used to recruit physical and occupational therapists from the University of Chicago Medical Center Inpatient Therapy Services department. In total, eight therapists agreed to participate, and seven were eligible to provide answers to our questions, based on their experience working in the hospital during the pandemic. A four-question semi-structured interview was developed to assess perceived differences between working before and during the pandemic and between working with COVID-positive and COVID-negative patients. Individual interviews were conducted using Zoom. Interviews were transcribed then coded using the constant comparative method.
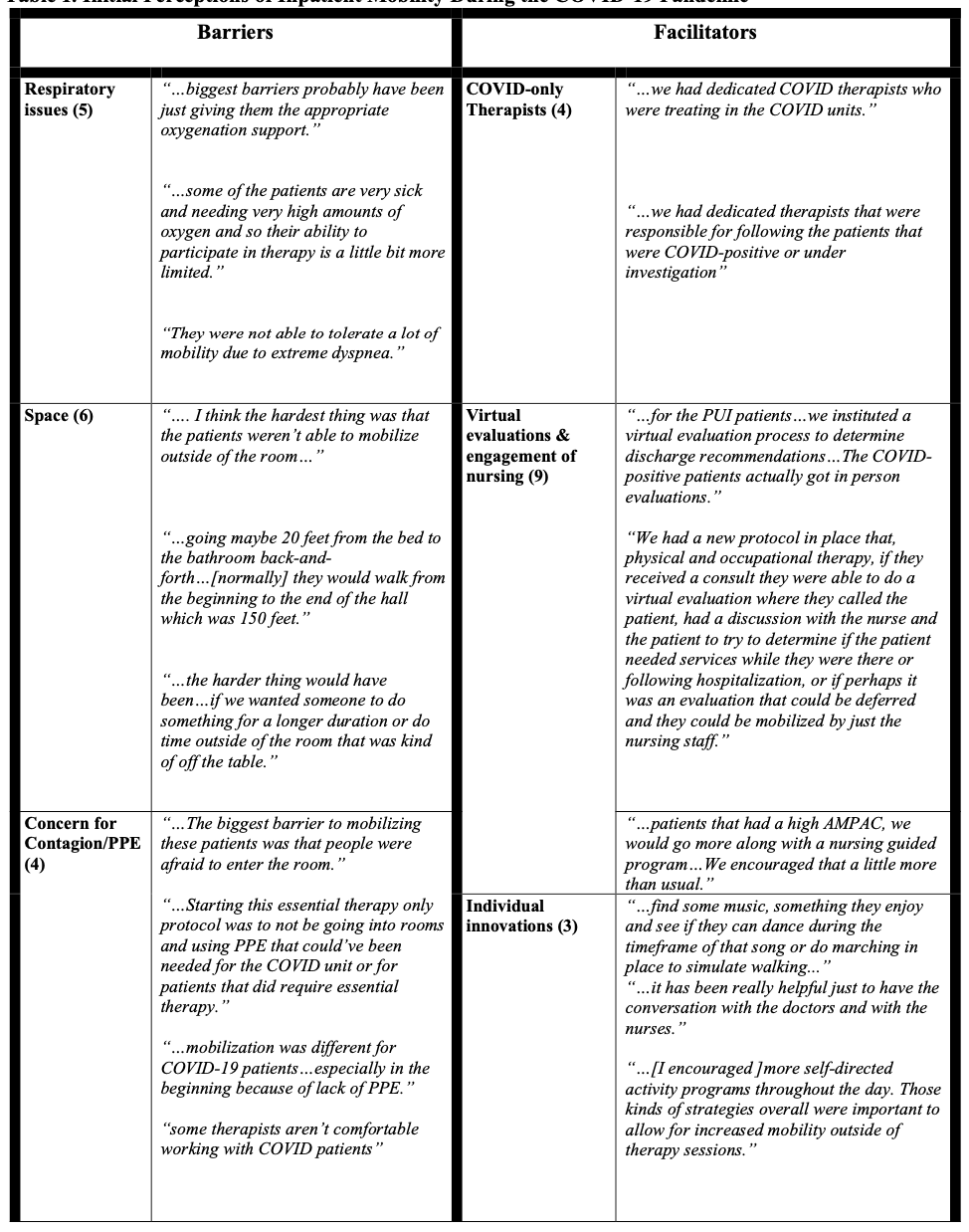
Results: Of the seven individual interviews that were analyzed, two main categories emerged: “barriers to therapy” and “facilitators of therapy”. Three sub-categories were identified within each of the parent categories. Subcategories of barriers to inpatient therapy included patient respiratory issues [n = 5], limited space to ambulate [n = 6], and concern for contagion/lack of PPE [n = 4]. Facilitators of inpatient therapy included designating specific therapists for COVID patients/patients under investigation [n = 4], implementing virtual evaluations and engaging nursing in mobilization (both were aspects of a new protocol implemented for the pandemic) [n = 9], and individual innovations such as preparation prior to entering a room or creative ways to encourage patients to ambulate [n = 3].
Conclusions: Additional barriers to inpatient physical and occupational therapy, including patient symptomatology and concern for contagion, have developed due to the COVID-19 pandemic. This increases the risk for HAD in patients hospitalized during the pandemic. However, rapid adaptation and innovation, from the hospital level to individual level, can be employed to overcome these barriers. Our team is currently recruiting nursing staff to assess nursing perspectives on this topic.