Case Presentation: This is a case of a 37-year-old female with a 9 month history of moderate ulcerative pancolitis (UC) who was admitted with worsening abdominal pain, a 30 lb weight loss, nausea, vomiting, and bloody diarrhea. She had been treated with mesalamine, vedolizumab, and infliximab with no improvement and refused corticosteroid therapy due to a history of being on steroids for 6 years for orbital myositis causing bilateral cataracts and significant weight gain. Stool culture on admission was positive for Aeromonas caviae complex, and she was treated with ceftriaxone followed by trimethoprim/sulfamethoxazole. For her UC, she was started on hyperbaric oxygen therapy with plans to start tofacitinib as an outpatient. After three days of ceftriaxone and two hyperbaric oxygen treatments the patient had some improvements in symptoms and significant improvement in CRP from 120 mg/l to 17 mg/l. Interestingly, nine months prior to her diagnosis of UC the patient developed profuse vomiting and non-bloody diarrhea after eating a poke bowl. Six days after her symptoms started, she presented to the ED for hydration and was found to have diffuse gastric hyperenhancement and cecal thickening on CT scan. While her vomiting resolved following this illness, her diarrhea and abdominal pain persisted until she was ultimately diagnosed with UC.
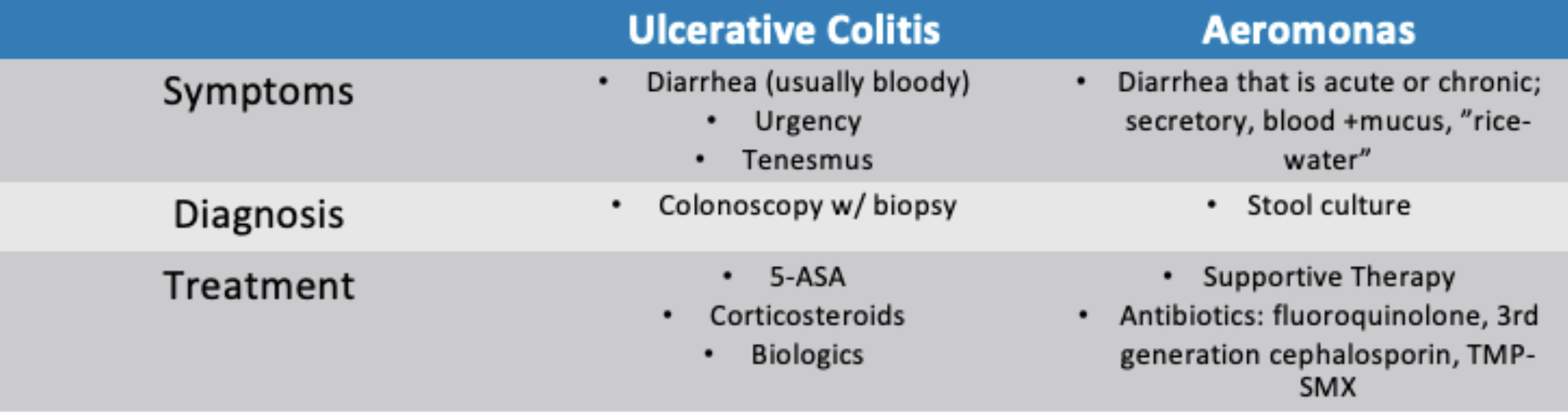
Discussion: Aeromonas infection generally causes an acute, self-limiting diarrhea, however some patients, especially the immunosuppressed, can develop chronic diarrhea with or without blood that may require antibiotic treatment. The role of Aeromonas infection in inflammatory bowel disease (IBD) is controversial and has been reported to trigger IBD flares or contribute to the development of IBD. This case is unique in that the patient has not achieved remission on multiple IBD medications, was resistant to steroids as typical UC flare treatment regimen, and had mild improvement in GI symptoms and significant improvement in CRP prior to discharge after initiation of antibiotic therapy, raising the question of Aeromonas possibly playing a role in her colitis, or whether it was an innocent bystander. Initiation of hyperbaric therapy and tofacitinib as an outpatient in addition to antibiotics makes it difficult to definitively draw a conclusion as to the cause of her improvement.
Conclusions: We propose that patients presenting with an IBD flare, particularly those with refractory disease, should receive a stool culture on admission to rule out infectious cause. Earlier recognition of infection in IBD patients allows for proper treatment of all potential drivers of infection.