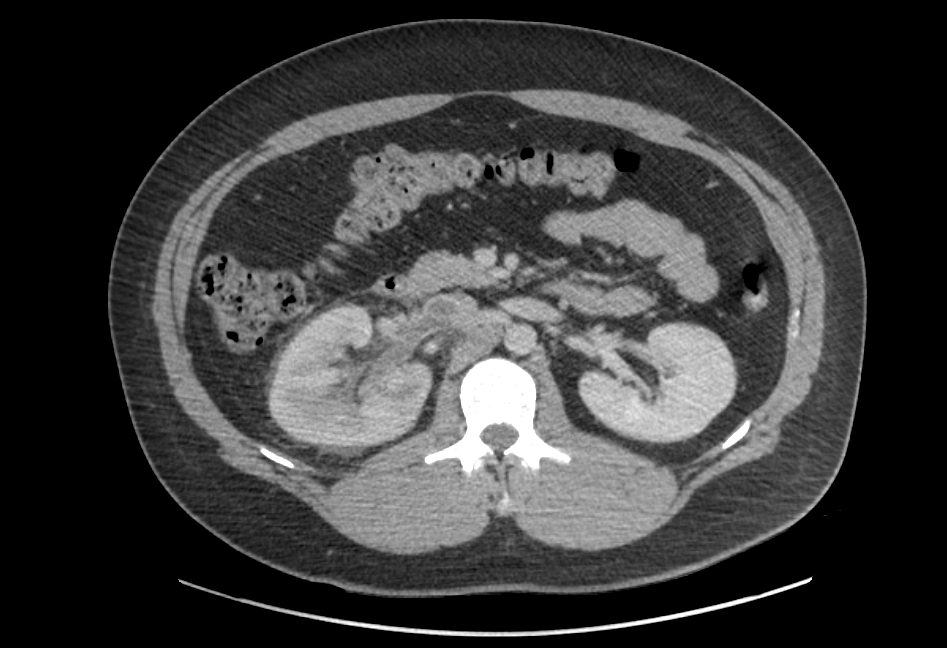
Case Presentation: Our patient is a 35-year-old male with a history of hypertension who was transferred from an outside hospital (OSH) for renal vein, and inferior vena cava (IVC) thrombosis. A month prior to presentation to the OSH, he had developed acute, right-sided flank pain with nausea. At the OSH, he was diagnosed with nephrolithiasis, and pyelonephritis, and was discharged on opiates, and ciprofloxacin. Following discharge, he experienced worsening flank pain, new testicular pain, (both on the right side), chest pain, and dyspnea. Repeat imaging at the OSH revealed a right renal vein thrombus extending to the IVC, bilateral pulmonary emboli, and an enlarged right kidney, with perinephric stranding. He was transferred to our hospital for further management. Pertinent labs in our hospital included an albumin of 2.1; total protein of 5.9; 3+ urine protein; and a 24-hour urine protein of 10.6 g. Antinuclear antibody, HIV, and hepatitis panel were negative. Renal biopsy revealed diffuse, subepithelial, electron-dense deposits, with diffuse effacement of podocyte foot processes. IgG4, and antibodies to phospholipase A2 receptor (PLA2R) were positive. He was diagnosed with primary MN, and started on cyclophosphamide, and prednisone for the MN, and rivaroxaban for the venous thromboembolism (VTE). At his one-month-follow-up visit, his proteinuria was sub-nephrotic, and he was being considered for cessation of anticoagulation.
Discussion: Almost all patients with MN initially present with nephrotic syndrome, as opposed to a small percentage, who are worked up for proteinuria noted incidentally. Our patient initially presented with dysuria, and flank pain. Retrospectively, however, his initial work up was noted to have revealed the presence of hypoalbuminemia; the absence of both pyuria, and calculi; negative blood, and urine cultures; and the presence of a mild filling defect in the right renal vein. A closer examination of his labs, and imaging, could have guided towards an earlier diagnosis of MN, with earlier initiation of treatment, and might have prevented the progression of the thrombus with the consequent extensive VTE.
Conclusions: There have, previously been, case reports published about MN, and the resultant nephrotic syndrome presenting initially as VTE. In our patient, however, the VTE of nephrotic syndrome secondary to MN masqueraded as infection. Given that in the absence of an anatomic abnormality, pyelonephritis in an adult male is an infrequent occurrence, the suspicion for noninfectious causes for such a presentation should remain fairly high. This case reiterates that it is of paramount importance to connect the dots while making a clinical diagnosis. While we, as physicians, never want to miss an infection, we would be remiss in having an incomplete list of differential diagnoses.