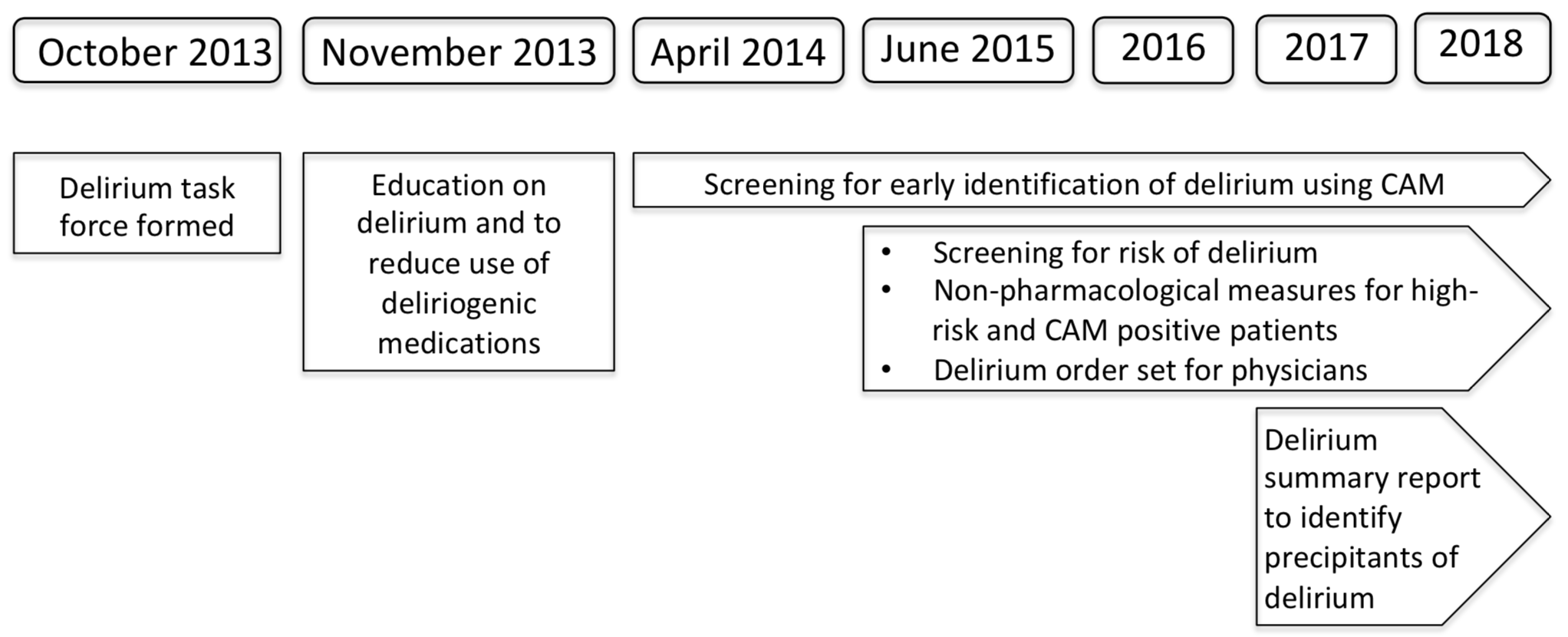
Background: Delirium is an acute change in mental status affecting 10-64% of hospitalized patients, and may be preventable in 30-40% cases. There was no standardized protocol for delirium at our hospital prior to 2014. In October 2013, we formed a task force for delirium prevention and early identification across 18 medical-surgical units in our hospital.
Methods: The objective of this initiative was to implement evidence-based strategies for delirium prevention and early identification as proposed in the literature. This is a retrospective cohort at a single academic medical center. We studied 105,455 patient encounters admitted between November 1, 2013 and January 31, 2018.
Since November 2013, there has been ongoing education to decrease the use of deliriogenic medications. Since 2014, nurses screen all patients for presence or absence of delirium using the confusion assessment method (CAM). A physician order set for delirium was created in 2015. Since 2015, nurses also screen all patients in whom delirium has not occurred, for risk of delirium. Non-pharmacological measures to prevent or manage delirium are implemented by nursing for high-risk or CAM positive patients.
We report: (a) Process measures: CAM screening at least twice daily, delirium risk screening once daily, and use of deliriogenic medications, (b) Primary outcome: Delirium rate among high-risk patients (N = 21,465), and (c) Secondary outcomes: Length of stay (LOS), inpatient mortality, and discharge to rehabilitation facility, among high-risk patients or those diagnosed with delirium (N = 22,121).
Results: 98.8% of the patient encounters had CAM screening, and 99.6% had delirium risk screening. The odds of use of opiates decreased by 5.0% per year, and the odds of use of benzodiazepines decreased by 8.0% per year since 2013. There was no change in the use of anticholinergics. In the adjusted analysis, the odds of delirium decreased by 25.3% per year among high-risk patients since 2015. Among high-risk patients or those diagnosed with delirium, the estimated LOS decreased by 0.13 days per year, the odds of inpatient mortality decreased by 16.0% per year, and the odds of discharge to rehabilitation facility decreased by 17.1% per year.
Conclusions: Hospitals are dynamic environments that evolve over time to accommodate the changing population and patient flow, new areas of clinical and financial focus, and changes in leadership. Quality improvement initiatives are particularly vulnerable to such changes. While there may be initial success, sustaining efforts and continuing to report and improve on them is far more challenging. With high clinician engagement and simple workflows, this initiative has shown sustained results, and may provide a reproducible model for other institutions.