Background: Physician burnout is a previously described and increasingly studied phenomenon that affects all fields of medicine to varying degrees. The Maslach Burnout Inventory (MBI) has been the historical gold standard for assessing burnout, but multiple new methods have been developed in recent years as greater attention is being paid towards physician wellness and burnout. In extension, there have been numerous attempts to design curricula and interventions to mitigate or reverse burnout, with varying levels of success. To date, there have been very few studies published of successful interventions specifically targeting hospitalist physicians. In this study, we seek to identify some of the primary determinants of hospitalist burnout, specifically as it pertains to the practice of hospital medicine throughout the novel Coronavirus pandemic.
Methods: A survey was disseminated to the hospitalists working at two tertiary referral hospitals in the Portland, Oregon region. Hospitalist physicians and nurse practitioners were asked to complete a survey regarding demographic information, job satisfaction, indicators of burnout, and their experience throughout the Covid-19 pandemic. This survey contained ordinal elements and provided space for tree-text responses. Participants at one hospital were similarly asked to complete the Maslach Burnout Inventory to provide quantitative information in several domains. For each question with ordinal components, data was analyzed to determine the mean, quartile distribution, and standard deviation. Free-text responses were reviewed by a group of investigators to identify common themes and potential avenues for targeted improvement.
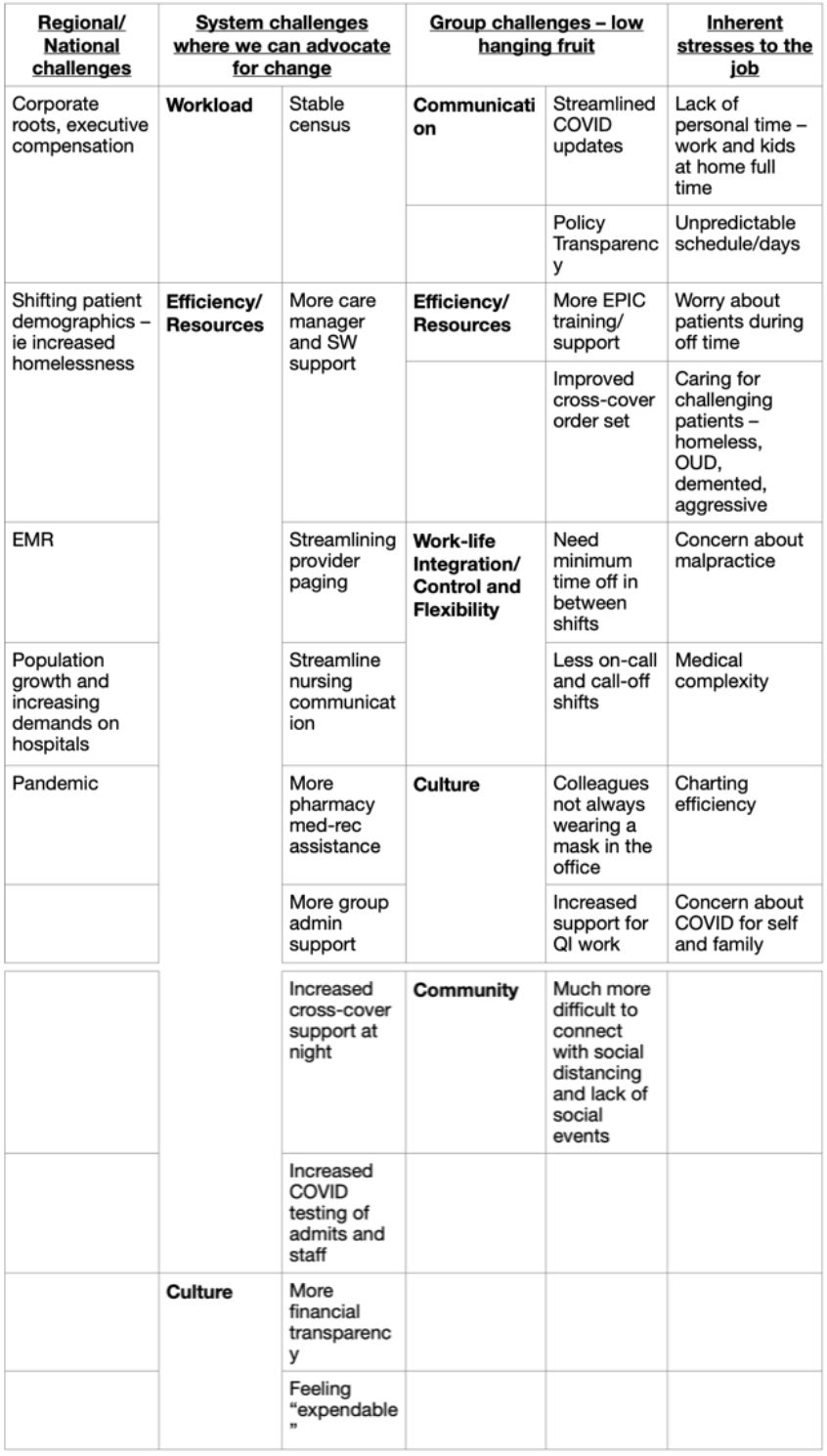
Results: 105 of 129 (81.4%) of requested surveys were completed and returned across the two hospitalist groups. Overall job satisfaction was high, with very few respondents having considered leaving their job or looking for alternative employment. Hospitalists did perceive, in descending order, significant health risks to their families, themselves, their colleagues, and their patients. Practitioners reported that the pandemic affected their healthcare organization more than it affected themselves. Of respondents who completed the Maslach Burnout Inventory, 19 of 52 (35.6%) endorsed high emotional exhaustion or depersonalization. This is markedly lower than the nationwide 54.4% rate reported in previous studies. Free-text responses were reviewed by a group of investigators with several categories and subcategories identified, with common responses collated (Table 1).
Conclusions: While hospitalists report that the Covid-19 pandemic has affected their professional lives and created substantial concern about the health risks to themselves and others, burnout rates in this group were below previously reported levels. Using qualitative data, we were able to create a framework to help move concrete interventions forward to improve burnout and job satisfaction for one Hospitalist group.