Background:
It is estimated that 7%–15% of all strokes occur in the hospital, yet these strokes have slower response times and longer time to thrombolysis compared with strokes that occur outside the hospital. We initiated an inpatient stroke alert program to improve in‐hospital stroke recognition and reduce time to evaluation.
Methods:
The University of Colorado Hospital initiated the program October 1, 2006. Prior to this, the stroke alert system existed primarily for the emergency department (ED), with stroke team involvement in in‐hospital strokes at the primary service's discretion. The new inpatient stroke alert protocol dictated direct activation of the stroke team by any hospital employee via a single alert number. An educational initiative on the signs, symptoms, and response to stroke was performed with all hospital staff. In a retrospective cohort analysis, we compared the 12 months before to the 12 months after program implementation in order to assess impact on in‐hospital stroke response time (defined as time from symptom recognition by medical staff to any brain imaging).
Results:
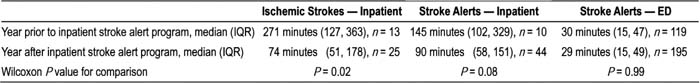
In the year prior to the program, there were 10 in‐hospital stroke alerts, of which 7 were true ischemic strokes. Administrative coding data identified 6 additional in‐hospital ischemic strokes in which the acute stroke team was not involved. In the year after program implementation there were 44 in‐hospital stroke alerts, of which 22 were true ischemic strokes. Administrative coding data identified 3 additional in‐hospital ischemic strokes. Stroke alerts occurring in the ED were not targeted by this intervention, and there was no change in ED stroke alert response time after implementation of the in‐hospital stroke alert program (30 versus 29 minutes, P = 0.99). ED stroke alert response times across the study period were significantly shorter than for in‐hospital stroke alerts (29 versus 98 minutes, P < 0.0001). There was a trend toward reduced response times for all in‐hospital stroke alerts (median 145 versus 90 minutes, P = 0.08) after program implementation. There was a significant decrease in response time for true ischemic in‐hospital strokes, from a median of 271 minutes to a median of 74 minutes (P = 0.02) after program implementation. The percentage of in‐hospital ischemic strokes with stroke team activation increased from 54% (7 of 13) to 88% (22 of 25), although the false‐positive alarm rate rose from 30% (3 of 10) to 50% (22 of 44).
Conclusions:
This inpatient stroke alert program significantly reduced response time for in‐hospital ischemic strokes. It increased stroke team recognition of in‐hospital strokes, although at the cost of an increased false alarm rate. Inpatient stroke response times were significantly longer than ED stroke response times, and this is a target for further investigation.
Author Disclosure:
E. Cumbler, none; T. Anderson, none; R. Neumann, none; W. Jones, none; K. Brega, none.