Background: A 2013 Mayo Clinic initiative (Henkin et al, 2016) to encourage communication between physicians and nurses by paging each to bedside for daily morning rounds improved physician and nursing perceptions of teamwork. Utilizing a mobile electronic-health-record-based alert for such a process has the potential to reduce implementation cost and feasibility barriers but has not been trialed.
Purpose: Our primary objective was to implement an updated interprofessional bedside rounds (IBR) model that utilized secure-texting platform alerts in order to improve attending, resident and RN communication and satisfaction on general medicine services at an academic hospital.
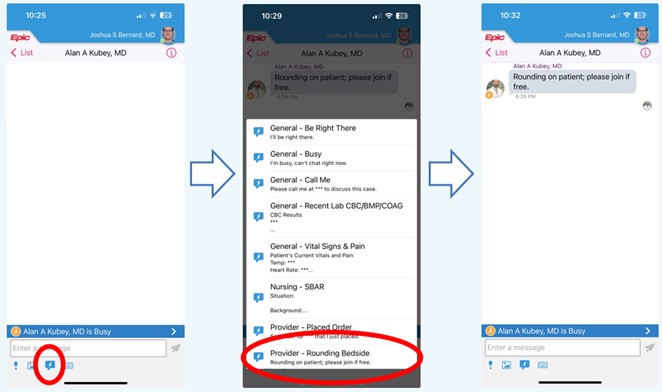
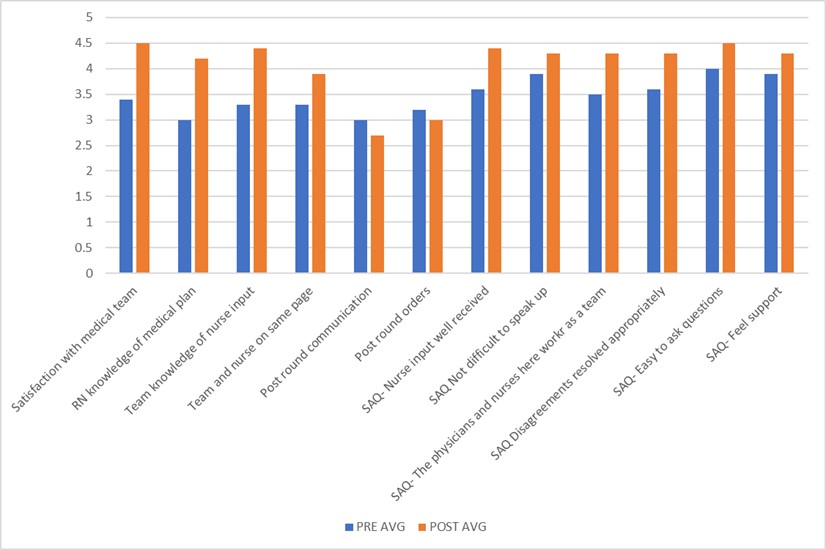
Description: Participants included volunteer hospitalist attendings and advanced-practice providers (APPs), the residents on those teams and nurses for patients on a single med-surg/telemetry hospital unit. A multidisciplinary executive committee developed expectations and communicated process expectations via email, secure-texting platform, and in person. The expectation was that the medical team would send a pre-populated secure-text to alert the primary nurse to bedside rounds. The nurse would then advise the medical team regarding (1) any questions/concerns and (2) any orders needed and the medical team would advise the nurse of the general plan for the day (Figure 1). The goal was for this interaction to last < 1 minute. Participants were surveyed before and after the intervention across twelve domains with a 5-point Likert scale (1- do not agree at all, 5- completely agree): team-nurse communication satisfaction, medical plan knowledge, burden of post-rounds unnecessary communications and orders, and the six-question Safety Attitudes Questionnaire (SAQ).Using matched pre-post survey analysis (49% [33/68] post response rate), all twelve domains showed trends toward improvement (nine were significant). The average pre-post response increased from 3.5/5 to 4.3/5. Specifically: satisfaction with medical team-RN communication and collaboration increased 1.06 (95% Confidence Interval [95% CI]: 0.75-1.38, p< 0.0001); RN knowledge of medical plan 1.2 (95% CI 0.82-1.56, p< 0.0001); team knowledge of nursing input 1.13 (95% CI: 0.72-1.53, p< 0.0001); team and nurse are on the same page 0.69 (95% CI: 0.33-1.04, p=0.0007); SAQ-nurse input well received 0.82 (95% CI: 0.51-1.13, p< 0.0001); SAQ-not difficult to speak up 0.42 (95% CI: -0.04-0.88, p=0.08) SAQ-physician-nurses work together as a well-coordinated team 0.73 (95% CI: 0.45-1.0, p< 0.0001); SAQ-disagreements are resolved appropriately 0.64 (95% CI: 0.34-0.93, p=0.0002); SAQ-easy to ask questions 0.54 (95% CI: 0.29-0.80, p=0.0002); SAQ-have support from other personnel to care for patients 0.39 (95% CI: 0.13-0.66, p=0.007); post-round calls/secure chats -0.3 (95% CI: -0.76-0.38, p=0.31); post-round orders -0.3 (95% CI: -0.58-0.30, p=0.23), respectively (Figure 2).
Conclusions: IBR through EHR-based notification improves both provider and nursing communication and satisfaction with promising trends in reduced unnecessary/disruptive post-rounds communication and orders.