Background: Hospital discharge is a vulnerable moment in healthcare delivery that impacts patient safety and experience. Improving this care transition necessitates a focus on the most error-prone and potentially hazardous parts of the process, including discharge logistics (e.g., transportation), medication safety, follow-up plans, and contingency planning. Many interventions have been investigated to improve discharge processes; however, most fail to simultaneously be interprofessional and nurse-driven and actively engage patients and their care partners.
Purpose: To pilot a nurse-driven interprofessional Discharge Huddle (DH); evaluate its effects on patient experience and engagement after discharge; and evaluate barriers to implementation and perceived impact based on stakeholder input.
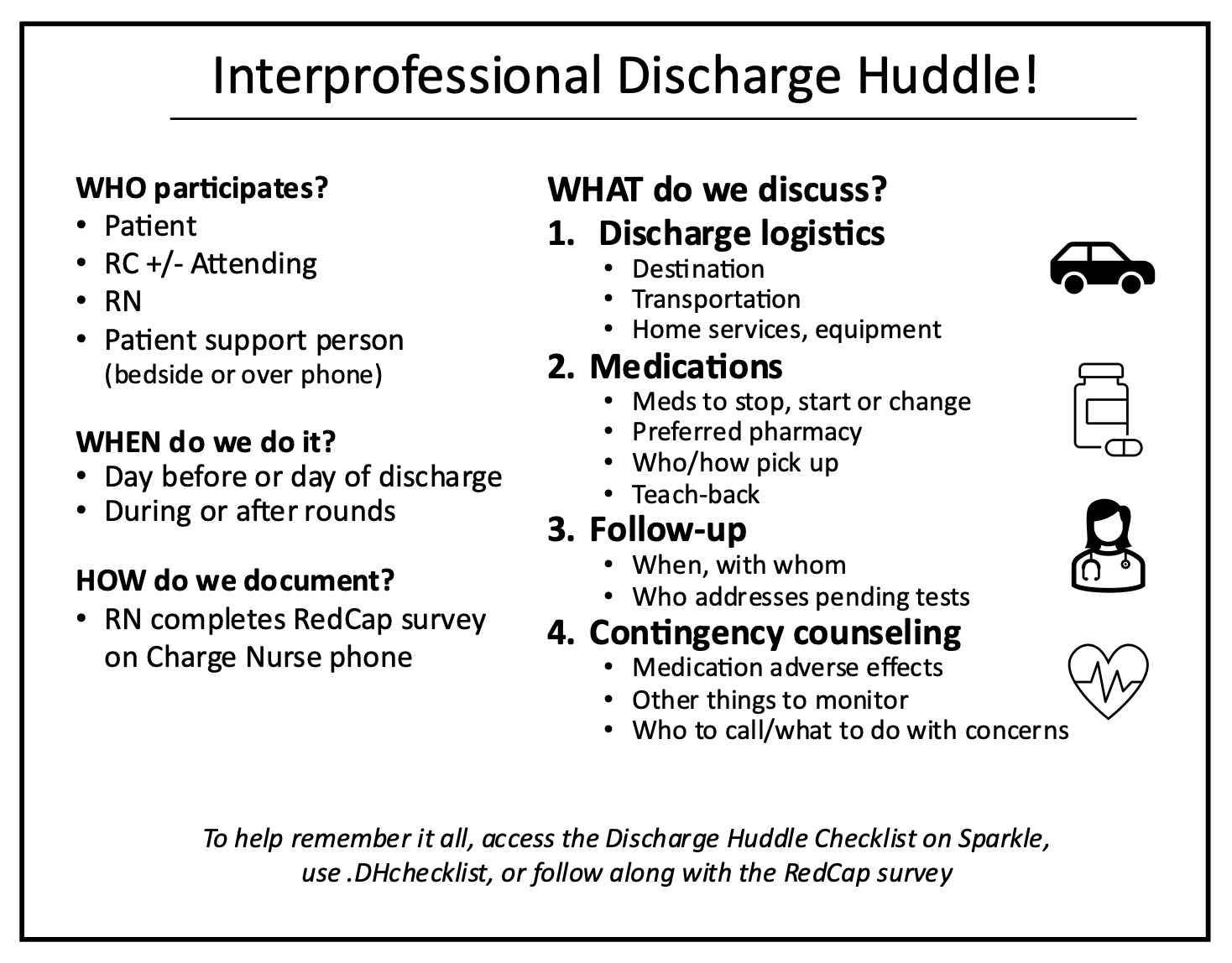
Description: The DH is a checklist-based discharge safety tool to collaboratively review discharge logistics, medication changes, follow-up plans, and contingency planning with the nurse, resident, patient, and a patient support person (either in person or by phone) (Figure 1). It was designed by an interprofessional workgroup (hospitalists, nurses, and residents) and piloted as a mixed methods quality improvement project on a general medicine teaching service from 5/2023 to 8/2023. Resident teams and nurses were taught about the DH at orientation sessions and staff meetings, an informational DH poster was placed throughout the unit and made available on a mobile application, and providers received email reminders regarding the DH from unit nursing and hospitalist leadership. Primarily nurses organized the DHs and documented completion via a REDCap survey that was also designed to facilitate DH execution. During the study period, 59 DHs out of 249 eligible discharges were documented, the majority (69%) of which occurred during the first month of the pilot. 21% of documented DHs identified a new issue with the discharge plan, mostly commonly related to medication reconciliation or the follow-up plan. During the month of highest DH utilization, there was a trend towards greater patient satisfaction on routinely administered post-discharge surveys (top-box responses from 77-83% vs. 56-67% of survey responders the same month the previous year), and a trend towards a greater proportion of follow-up appointments attended among patients admitted to the study service compared to a usual-care general medicine service on different hospital units (21% vs. 15% with a completed appointment and no cancellations). Qualitative measures included nurse testimonials and semi-structured focus groups with residents and hospitalists (Table 1). Nurses consistently felt the DH improved communication around discharge, facilitated smooth discharge workflow, and was appreciated by patients. Common barriers to implementation were workflow/logistics, insufficient training, and lack of time.
Conclusions: In this mixed methods pilot study, use of an interprofessional, nurse-driven Discharge Huddle was associated with improved nurse perceptions of discharge communication and workflow and demonstrated a trend towards greater patient satisfaction and completion of follow-up appointments based on preliminary data. Interpretation of these data is limited by small sample size and variable DH completion across the study period. However, the DH is promising, and more comprehensive implementation with enhanced provider training is warranted to assess its full impact.