Background: Perioperative hyperglycemia is associated with poor surgical outcomes, including infection and mortality, with higher rates of complications in patients without diagnosed diabetes (NDM) than in those with diabetes. Insulin therapy has been found to decrease the risk of infection and other adverse outcomes following surgery. It is unclear, however, whether insulin therapy for hyperglycemia improves neurologic outcome following neurosurgery. The aim of this study was to examine the relationship between perioperative glucose control and adverse outcomes among patients undergoing intracranial procedures.
Methods: Data was collected from a single academic institution, retrospective cohort, from May 2012 through May 2017. Included patients who underwent an intracranial procedure, had a length of stay of at least 48 hours, and were at least 19 years of age. Data collected include demographic and baseline characteristics, length of stay, perioperative administration of steroids and insulin, and perioperative blood glucose measures.
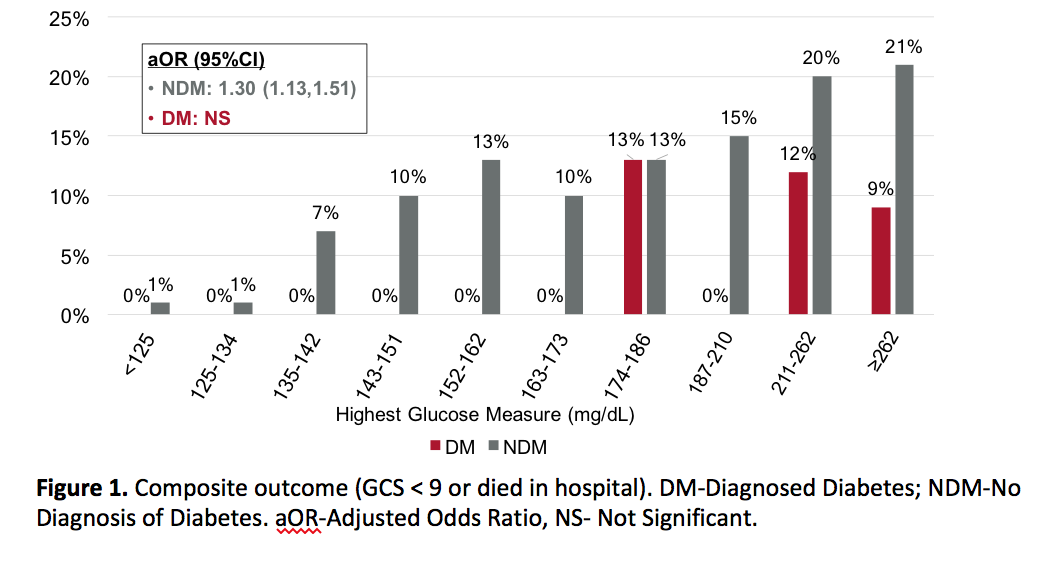
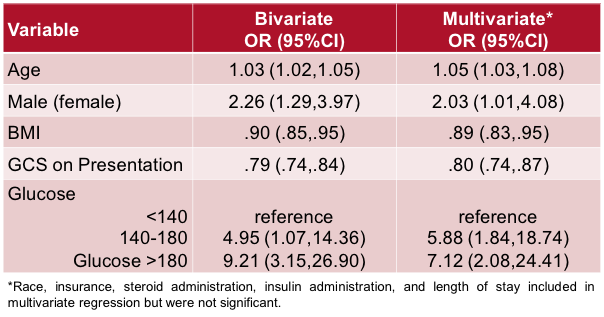
Results: Increased glucose measures were associated with increased poor outcomes in NDM patients, but not in patients with diabetes (Figure 1). Among NDM patients, only 46% of patients with severe hyperglycemia were administered insulin, compared to 90% of patients with diagnosed diabetes. In a multivariate model, NDM patients with moderate hyperglycemia were almost six-fold more likely, and those with severe hyperglycemia were seven-fold more likely to discharge with low GCS or die in hospital (Table 1).
Conclusions: Hyperglycemia was associated with poor outcomes for NDM patients; but not for patients with diabetes. Of note, NDM patients were significantly less likely to receive insulin in the setting of hyperglycemia, compared to those with diabetes. This suggests that increasing attention to perioperative glucose monitoring and appropriate intervention could alter outcomes for NDM patients undergoing intracranial surgery.