Background: Nearly half of incorrect procedures occur outside the operating room, and failure to conduct a robust time-out is a frequent root cause. Mannequin-based simulation (MBS) has been shown to improve self-confidence and performance of time-outs, but is expensive, time-consuming, and difficult to scale up effectively for large groups of medical learners. Screen-based simulation (SBS) represents a cost-effective alternative learning platform capable of reaching an unlimited number of learners. This study poses the following research question: How does MBS versus SBS impact the learning outcomes for curricula that teach time-outs for invasive procedures outside the operating room?
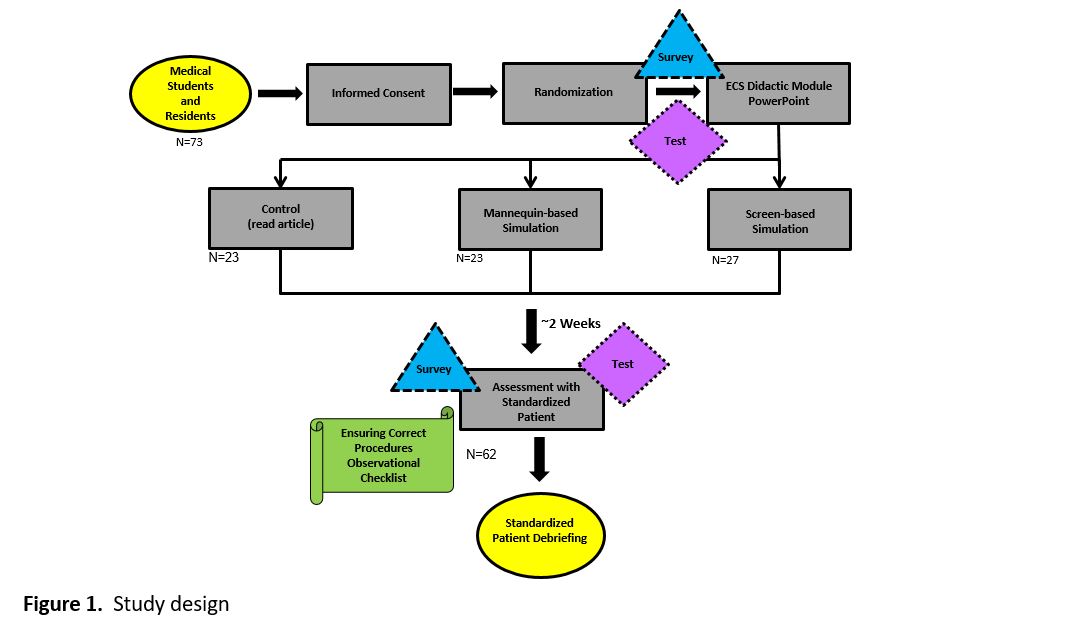
Methods: Medical students and residents completed a baseline confidence survey and knowledge test followed by a brief didactic on time-outs. They were then randomized to control, MBS, or SBS groups. Control learners read an article. MBS participants engaged in a thoracentesis time-out simulation with an instructor and debrief. SBS participants completed an online, interactive thoracentesis time-out case scenario on an iPad. Two weeks later, participants repeated the survey and completed a time-out test simulation with a standardized patient (Figure 1). Tests were video recorded and performance was evaluated by two trainers using a validated 10-point observational checklist.
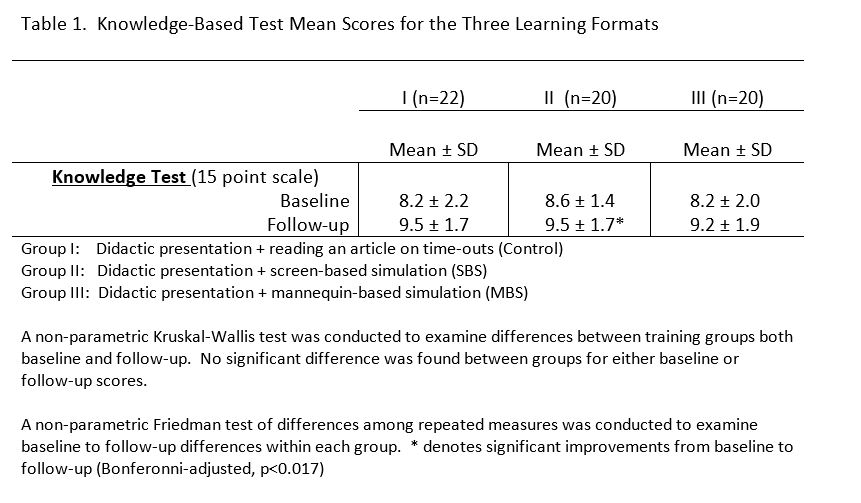
Results: Sixty two participants were distributed randomly amongst the MBS (20), SBS (20), and control (22) groups. MBS produced the highest mean score on the observational checklist at 8.35, with SBS and the control group scoring 7.15 and 6.5, respectively. As outlined in Table 1, baseline knowledge testing was comparable for all three groups, however, SBS was the sole format demonstrating an improvement in knowledge (8.6 to 9.5, p<0.017).
Conclusions: This study reaffirms that high fidelity simulation-based training (like MBS) can effectively address the challenge of wrong site invasive procedures outside the operating room. Although SBS did not demonstrate as strong a learning impact as MBS, it trended toward a similar result when compared with controls. Furthermore, it was the only group to produce a significant improvement in knowledge, and is attractive due to its easy scalability, flexibility of administration time/venue, and low trainer effort. We strongly believe that with further development, SBS can provide performance results comparable to or beyond MBS. We advocate for further exploration of SBS methods by both medical education and simulation faculty, as it can be applied to numerous other learning topics as well.