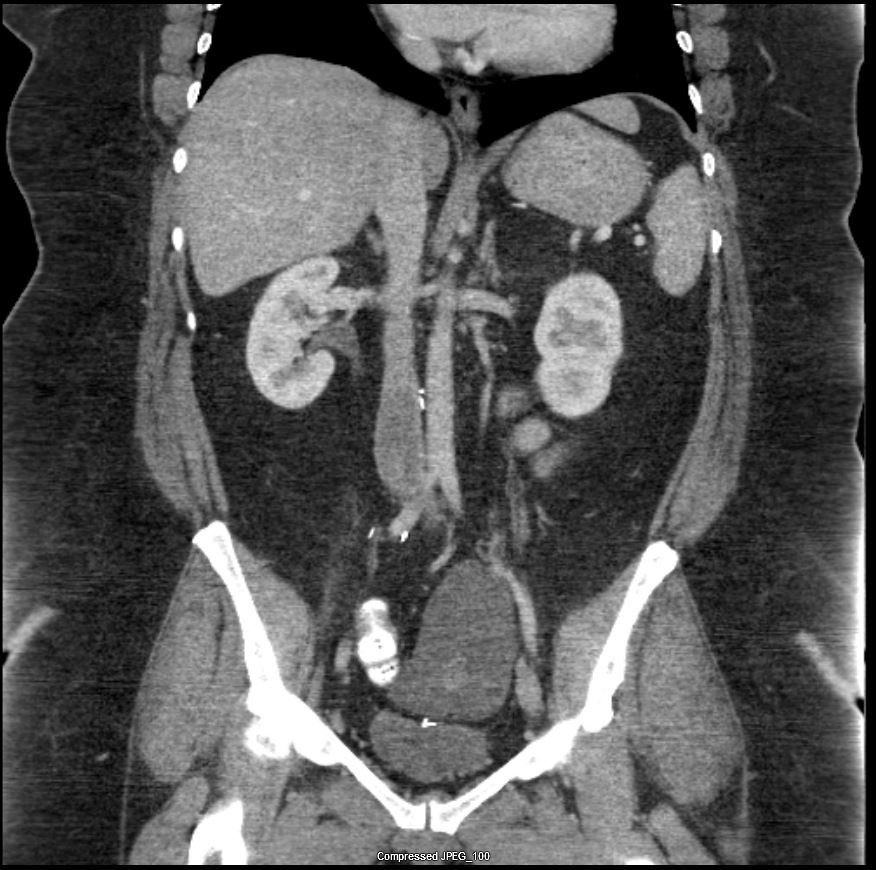
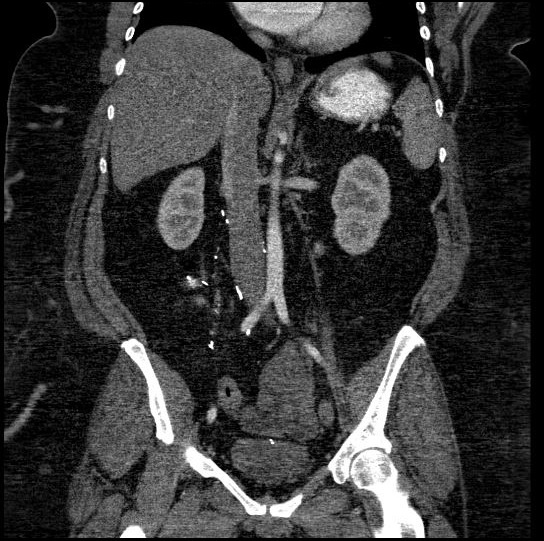
Case Presentation: A 43-year-old woman was admitted to the hospital for increasing lower extremity swelling and dyspnea on exertion. Past medical history is pertinent for hypertension, obesity, and stroke. A few months prior, she had a hysterectomy for leiomyomata. Physical examination was within normal limits except for jugular venous distension and irregular heart rate and rhythm. Transthoracic echo revealed reduced ejection fraction of 20-25% and a 4.0 x 3.5 cm globular mass, almost filling the entire right atrium. CT scan of the chest, abdomen, and pelvis reported on extensive IVC thrombus extending contiguously from the right mid external iliac vein and the left common iliac vein through the IVC and into the right atrium, in addition to a lobulated 12 cm pelvic cystic mass. The patient underwent successful right atrial, IVC, and bilateral iliac tumor thrombus resection and the patient was later discharged. Subsequent thrombus pathology described angioleiomyoma, and pelvic mass histopathology reported benign leiomyoma. One year later, the patient noticed the recurrence of the dyspnea on exertion and lower extremity swelling. Workup revealed new pulmonary nodules on chest CT scan which led to the diagnosis of benign metastasizing leiomyoma (BML). Transjugular IVC mass biopsy performed, and pathology was consistent with intravascular leiomyomatosis (IVL) with ER+/PR+ on immunohistochemical stains. Preoperative TTE showed 15-20% LVEF for which, the patient deemed a poor candidate for surgery and thus, hormonal treatment with leuprolide and letrozole started. While on this treatment, her abdominal mass and lung nodules were considered stable by RECIST 1.1 criteria (9.2% decrease in total tumor burden size), and she has had no new symptoms for the last 2 years. Genetic testing showed amplification of JUN, cyclin-dependent kinase 4 (CDK4), and MCL1, and loss of SUFU, AT-rich interaction domain 1A (AR1D1A), RB transcriptional corepressor 1 (RB1), and Hepatocyte nuclear factor 1-alpha (HNF1A).
Discussion: BML is a rare condition, first described in 1939. It is usually diagnosed several years after hysterectomy for uterine leiomyoma. IVL is a rare, classically benign uterine smooth muscle cell tumor that extends into the venous system. IVL arises from the tunica media of the veins and could potentially cause an intraluminal thrombus which may extend to the right heart through the pelvic veins and IVC. Treatment of pulmonary BML depends on the extent of the disease, the expression of estrogen and progesterone receptors in the tumor which makes them responsive to hormonal manipulation, and the age of the patient, it may include hysterectomy with oophorectomy, debulking surgery and/or the use of GnRH agonists, aromatase inhibitors, selective estrogen receptor modulators, or chemotherapy to decrease tumor burden in conditions that are unamenable for surgery.
Conclusions: This unique case represents a novel approach to the study of BML, supporting that genetic studies could be useful in providing a further understanding of this tumor’s mechanism of metastasis. Here, we discussed the molecular profiling results of intravascular leiomyomatosis, which showed amplification of CDK4, JUN, and MCL1 loss, besides, we identified amplification of AR1D1A, RB1, SUFU, and HNF1A loss. These findings may suggest molecular evidence of the malignant behavior of a previously thought benign entity.