Background: Hospitals continue to experience pressures to optimize efficiency and quality outcomes and to reduce practice variation. In surgical patient populations, the Enhanced Recovery After Surgery (ERAS) pathways have been shown to reduce length of stay, postoperative complications, hospital readmissions, and cost by integrating multidisciplinary, evidence-based interventions throughout the perioperative period (1). A similar model does not currently exist for general medical patients.
Purpose: To develop a framework of hospital-based best practices that can be applied to a heterogeneous population of general medical patients to advance their care safely and efficiently from admission through discharge.
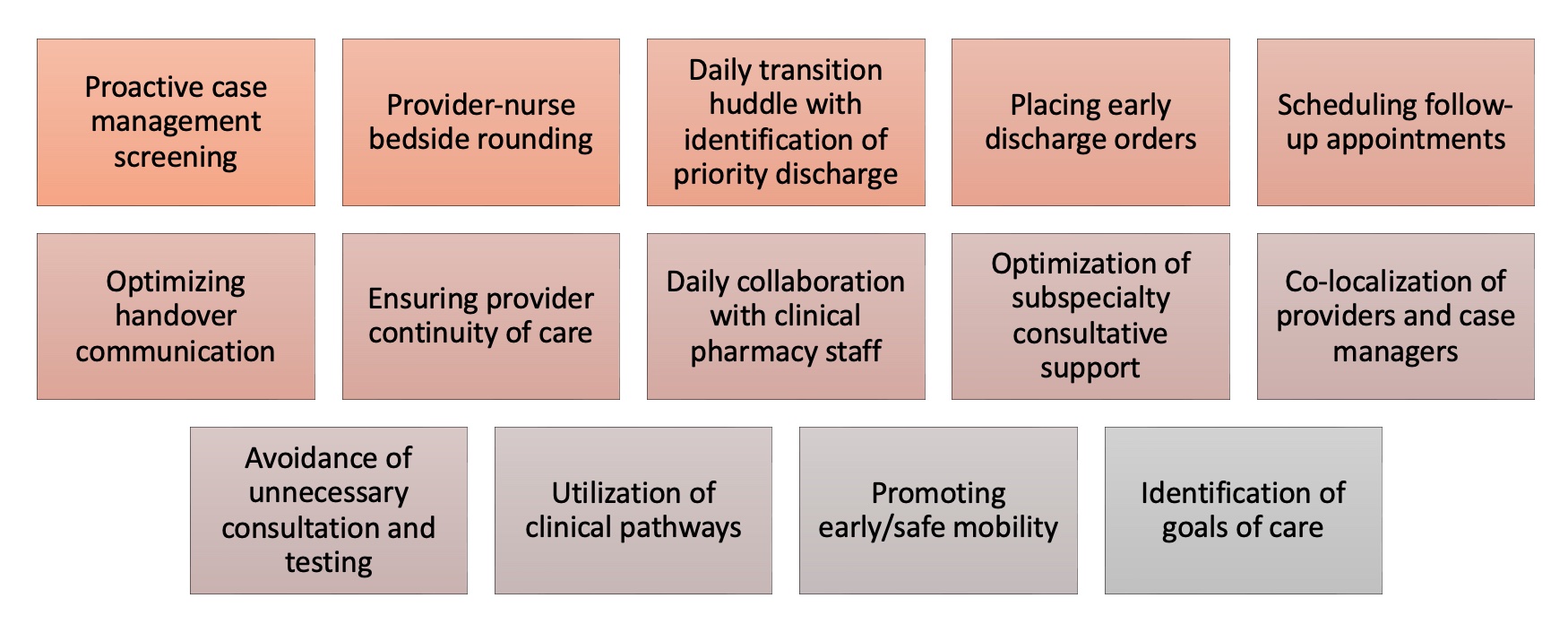
Description: Using lessons learned from the ERAS program and best practices from the literature (2), we created the Enhanced Model for Medicine Admissions (EMMA). EMMA is comprised of 14 interventions and principles relevant to the care of hospitalized medicine patients that we sought to implement and coordinate among our hospitalist teams, inpatient units, and support departments (Figure 1). Some of these expectations, such as provider-nurse bedside rounding and early discharge orders, were part of larger institution-wide initiatives. Others, including handover communication and staggered scheduling of physicians and advanced practice providers, were local changes under our group’s direct control. The third group of interventions, such as co-localizing providers with case managers and promoting early mobility for patients, were managed as stand-alone process improvement projects. Multidisciplinary workgroups incorporating hospitalist leaders, nursing leaders, and other key stakeholders were responsible for defining goals, deliverables, and timelines, and for escalating barriers. Lagging metrics were aligned with hospital pillar goals around patient experience, quality, and finance. Leading metrics were identified to facilitate rapid-cycle improvement. Analytics and health information technology staff were engaged as needed to support measurement and reporting. The overall project was co-led by two hospitalist leaders with operational assistance from an administrative director. Implementation of the 14 EMMA initiatives took place on a rolling basis, rather than as a bundle that went live at one time (Figure 2). Notable barriers included engagement and accountability of hospital medicine clinical leaders, change management for busy frontline clinicians, coordinating efforts across disciplines, and timely analytics support for metrics and reporting. Measurement of impact on case mix index-adjusted length of stay, discharges before 11am, Press Ganey top-box scores, patient harm index, observed-to-expected mortality, 30-day readmissions, and provider/staff satisfaction is ongoing.
Conclusions: The Enhanced Model for Medicine Admissions, or EMMA, incorporates a multidisciplinary approach to implementing best practices for the care of hospitalized medical patients to standardize care and to improve efficiency and quality outcomes.