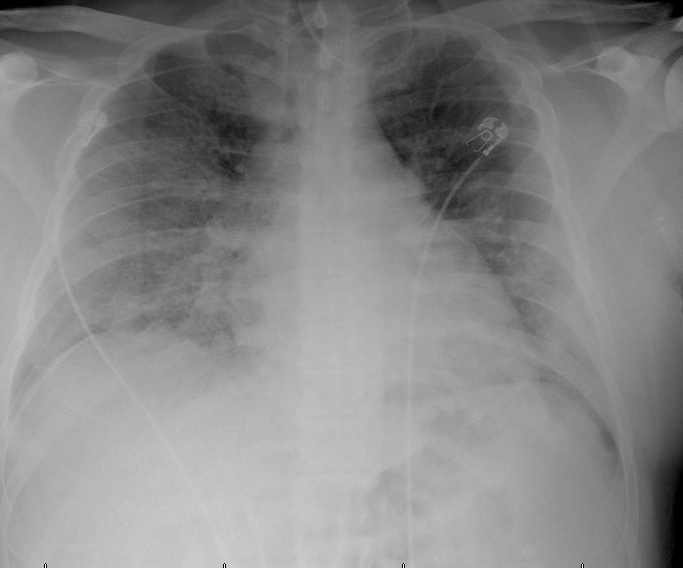
Case Presentation: A 41-year male with prior history of hypogonadism presented 11-days after positive COVIDtest with shortness of breath and no prior Covid vaccination. On presentation, patient wastachypneic with breathing rate 32/minute and was observed to be in acute hypoxic respiratoryfailure with oxygen saturation <50%, arterial blood gases showing Ph-6.93, partial pressure ofoxygen-53mmHg, and carbon-dioxide-85mmHg. Patient was immediately managed on Bi-levelpositive airway pressure ventilation showing improvement in oxygen saturation and blood gases.Laboratory investigations showed increased inflammatory markers with C-reactive protein-30.9mg/dl, procalcitonin-1.39ng/ml for which IV dexamethasone was started along with IVSarilumab-once along with venous thrombosis prophylaxis with enoxaparin. Eight hours afteradmission, patient complained of painful erection which apparently, he was experiencing since lastfive hours before notifying to the nurse. Urology was notified and immediately on examination,patient had 90-100% rigid corpora without glans tumescence. Parts prepared and penile block wasgiven immediately with 20ml of 1% Xylocaine. Left corporal blood was aspirated and confirmed withischemic priapism with Ph-6.82, partial pressure oxygen-40 and carbon-dioxide-110. Immediately,two 18-gauge needle inserted at base of penis into corpora bodies and dark blood aspirated. A totalof 2500mcg phenylephrine was injected into both corpora bodies after complete detumescence wasachieved and penis remained flaccid after procedure. However, 12hours after admission, priapismreoccurred and aspiration procedure was repeated. Priapism reoccurred 18hours after admissionwith third time occurrence and operative procedure with Al-ghorab shunt was planned. However,patient’s condition deteriorated and was intubated due to persistent low partial pressure of oxygenand altered mental status. About 24hours after admission, patient suffered cardiac arrest andunfortunately could not be revived.
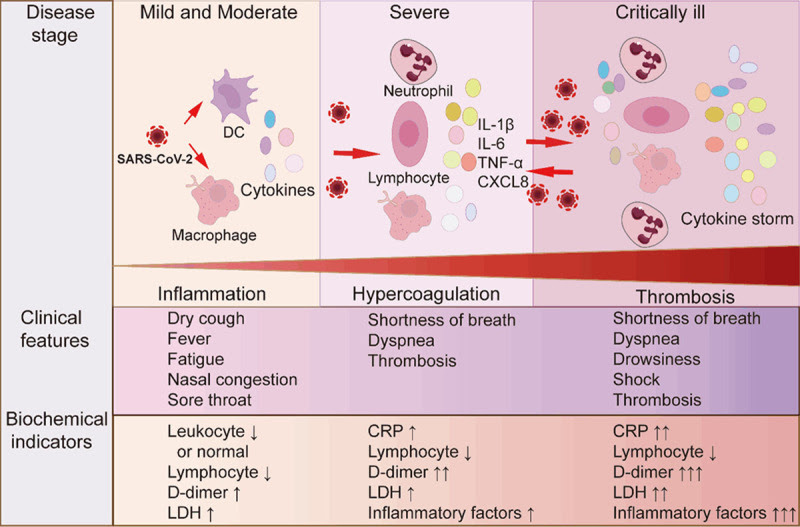
Discussion: Current literature review with less than ten case reports globally suggests associationbetween Covid induced inflammatory state with ischemic low-flow priapism. Prothrombotic statealong with endothelial dysfunction play a role in venous thromboembolism and obstruction of smallemissary veins. This theory is supported by findings such as dark, clotted and acidic blood onaspiration and recurrent ischemic priapism after multiple aspirations. Despite theoretical associationof thromboembolism and severe inflammation with ischemic priapism, no clear mechanism of onsethas been defined.
Conclusions: Rapidly deteriorating Covid-19 patients with high oxygen demands requiring Intensivecare are prone to complications like ischemic priapism. High clinical suspicion is necessary as its anemergent condition and timely treatment can prevent permanent damage and infertility. Most caseswere reported to have high inflammatory serum markers pointing towards prothrombotic state andreduced venous flow as the likely mechanism, however further studies are needed to establishpathophysiologic mechanism.