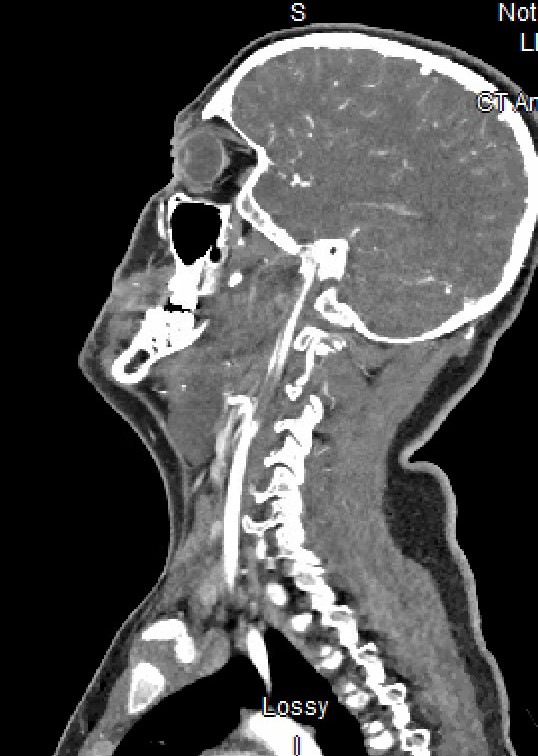
Case Presentation: A 15 year-old male with no significant medical history presented with fever, fatigue, headache, and neck pain with stiffness. His symptoms began several days prior to presentation and progressed to inability to fully move his neck, throat and jaw pain, and cognitive slowing. In the ED he underwent evaluation for infection and meningitis. He received empiric meningitic antibiotics and was admitted to the inpatient pediatric service. On exam the next morning, the team noted bilateral tonsillar hypertrophy, left greater than right, without uvula deviation. Additionally, the meningitis PCR panel returned negative. CSF cell count resulted with 250 WBC, 0 RBC, Protein 108, glucose 44. Due to suspicion of an indolent process other than meningitis, a CT soft tissue neck and head were obtained. Imaging showed a left parapharyngeal abscess extending to the jugular foramen causing significant narrowing of the left internal carotid artery as well as complete occlusion of the left internal jugular vein. CT angiogram of the neck and head evaluated for Lemierre’s syndrome (LS). It showed an epidural abscess, thrombosis of the left internal jugular vein to the left sigmoid and transverse venous sinuses, and a phlegmon surrounding the internal carotid artery causing severe vessel narrowing. Otolaryngology performed incision and drainage of the parapharyngeal abscess. Neurology, Interventional Neurology, and Hematology also consulted. Anticoagulation was started. The patient was discharged on an oral antibiotics and enoxaparin.
Discussion: The patient’s initial presentation was concerning for meningitis. However, the patient’s additional symptoms added deep neck space to the differential. The physical exam guided diagnostic evaluation. It is critical to be thorough with every new patient and analyze the working diagnosis to avoid anchoring bias or premature closure. The exam and tests resulted in the incidental discovery of Lemierre’s Syndrome and significant burden of infection and thromboses. LS predominantly affects children and young adults, with 90% of patients with reported LS to be between 10 and 35 years old (1). If not diagnosed and treated early, LS can result in prolonged hospital admission with ICU stay as well as progression to sepsis secondary to anaerobic infection, potential metastatic disease from septic emboli, and end-organ damage (2). Ultimately our further investigation allowed for the treatment of a potentially devastating infection before any long-term morbidity or mortality.
Conclusions: This case illustrates the importance of the physical exam in building a differential and guiding management. Anchoring and premature closure can be minimized by careful physical exam and analysis of lab results. Lemierre’s syndrome is uncommon but must always be considered in deep neck space infections given potential for increased morbidity and mortality