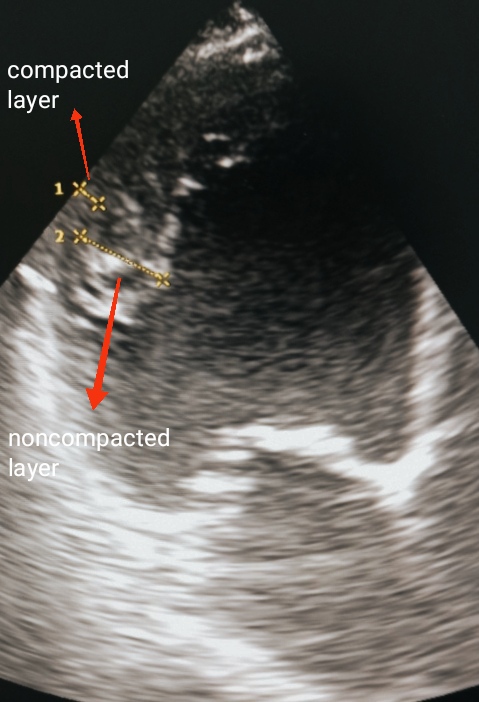
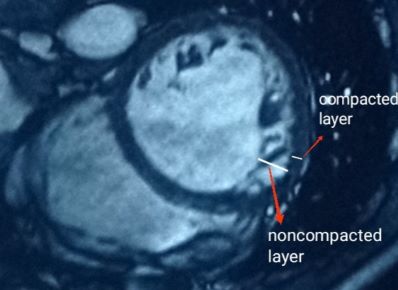
Case Presentation: A 62-year-old white male, without significant past medical history or risk factors, was referred to our clinic for arrhythmia evaluation. The patient had several brief episodes of palpitations for the last two months. On physical examination blowing systolic murmur at the apex and irregularly irregular rhythm were noticed. The 12-lead ECG demonstrated atrial fibrillation and ST-T segment depression in the V4-V6 leads. Transthoracic echocardiogram (TTE) showed signs of dilated cardiomyopathy with enlarged left cardiac chambers, severe eccentric LV hypertrophy, decreased contractility (EF< 30%), moderate mitral and tricuspid regurgitations, moderate pulmonary hypertension. Multiple prominent trabeculations were noticed in the middle and apical segments of the left ventricle. A non-compacted to compacted myocardium ratio was > 2.3 : 1. Cardiac catheterization excluded ischemic heart disease. Cardiac magnetic resonance (CMR) imaging confirmed the diagnosis. The patient was prescribed heart failure medications. ICD implantation was recommended.
Discussion: Isolated left ventricular noncompaction cardiomyopathy (LVNC), also known as spongy myocardium, is an extremely rare congenital disorder, belonging to unclassified cardiomyopathies by the World Health Organization, and classified as a genetic cardiomyopathy by the American Heart Association. Adult prevalence is 0.017–0.26% in observational echocardiographic studies with a 3:1 male:female ratio [1,2,3]. The disease occurs due to intrauterine arrest of normal myocardial compaction, resulting in prominent trabeculae, deep intertrabecular recesses, and thickening of the myocardium due to non-compacted layer, leading to left ventricular (LV) dysfunction. Predominantly the apical, mid-inferior and mid-lateral walls of the left ventricle are involved. Knowledge regarding proper diagnosis, morbidity and prognosis is limited, thus, this disease is mostly missed in adult patients. Reported mortality is high, ranging from 35-47% over a 42- to 72-month follow-up period [4]. Establishing a diagnosis of LVNC in elderly patients is challenging due to presence of other acquired cardiac diseases, including ischemic heart disease, hypertension, and other comorbidities, presenting with similar symptoms. Our aim is to highlight a diagnostic approach to LVNC in an elderly patient, making the disease more recognizable.
Conclusions: In conclusion, the diagnosis of LVNC in an adult population is often delayed because of similarities with more frequently diagnosed diseases. TTE is the initial diagnostic test of choice. Using strict echocardiographic Jenni et al., Chin et al., Stollberger et al. criteria we can increase identification of this condition. However, multiple diagnostic modalities (contrast echocardiography, MRI, genetic testing) may be required for complete assessment. Early diagnosis is crucial, because of the high incidence of life-threatening complications, related to heart failure, thromboembolic events and ventricular arrhythmias. Additional prospective studies are needed to improve management and outcomes of this rare cardiomyopathy.