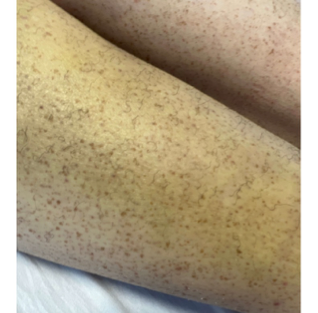
Case Presentation: A 29-year-old woman with a history of two first trimester losses, spontaneous hematoma and deep vein thrombosis was hospitalized for the management of acute anemia. Six weeks prior, she was hospitalized for a spontaneous right calf hematoma. Four weeks later, she was diagnosed with an unprovoked acute right popliteal vein thrombus and was initiated on an infusion of unfractionated heparin, complicated by anemia, requiring 5 units of packed red blood cells transfusion over several days. She left against medical advice and presented to a tertiary care center for further evaluation. On readmission, her physical examination revealed gingival bleeding, diffuse non-palpable purpura and petechiae, with tender right lower extremity, swelling and hematoma. Hemoglobin was 6.1 g/dL with leukopenia of 2.62 K/cu mm. Haptoglobin and lactate dehydrogenase were normal. Direct antiglobulin test was negative. Absolute reticulocyte count was elevated at 241.1K/cu mm. Vitamin K level was low at 54 pg/mL. Diluted Russell Viper Venom Time and anticardiolipin IgM were mildly elevated to 59.7 s and 21 standard units respectively. Computed tomography showed no source of bleeding.A dietary history was notable for multiple prior anaphylactic reactions after eating fruits, which she has eliminated from her diet. She also avoided vegetables due to preference. She was diagnosed with scurvy (vitamin C deficiency) given exam findings of follicular hyperkeratosis and coiled hairs (figure one), dental caries (figure two), and anemia. She was further diagnosed with Vitamin K deficiency as the likely etiology of her bleeding. Her deep vein thrombosis was managed with inferior vena cava filter placement due to multiple failed attempts at anticoagulation. She was empirically initiated on ascorbic acid 500 mg daily, and at follow up four weeks later, her petechia, leukopenia and anemia had resolved. She was also referred to follow up at allergy clinic.
Discussion: A micro-nutrient poor diet with the constellation of symptoms of extensive hematoma, generalized petechiae, gingival bleeding and persistent anemia are suggestive of scurvy. Although Vitamin C levels were not tested as ascorbic acid levels are not reliable determinants of functional vitamin C status, all symptoms improved with initiation of vitamin C supplementation, making the diagnosis of scurvy very likely. Risk factors for scurvy include alcoholism, low socioeconomic status (inability to afford fruits and vegetables), and severe psychiatric illness leading to poor nutrition1. When diagnosis is made promptly, the treatment consists of Vitamin C dosing ranged between 250 and 2000 mg daily. The prognosis is generally good, with complete resolution of presenting symptoms by an average of 3 months. However, acute unprovoked deep venous thrombosis is not typically seen in cases of scurvy. Therefore, we suspect an underlying diagnosis of anti-phospholipid syndrome, as increased oxidative stress (such as seen in Vitamin C deficiency) has been associated with both atherothrombosis and anti-phospholipid syndrome2. Although the patient did not meet diagnostic criteria, repeat anti-phospholipid syndrome testing would be indicated.
Conclusions: Although scurvy is rare in developed countries, it is an important diagnosis to consider in at-risk patients presenting with perifollicular hyperkeratosis and gingival hemorrhage. It is also important to assess for additional nutritional deficiencies (such as vitamin K for our patient) when one is found.